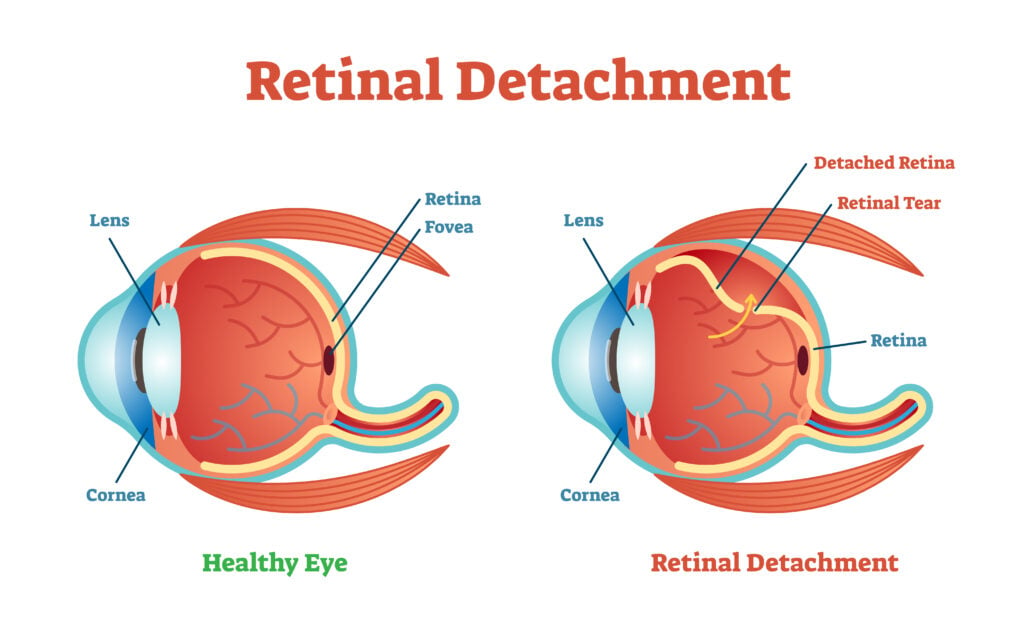
Retinal detachment occurs when your retina, the layer of tissue at the back of your eye, peels away. It's an urgent condition because the longer your retina remains detached, the greater the risk of permanent vision loss.
In this article, we’ll go over everything you need to know about retinal detachment and why it needs immediate medical attention.
What Causes Retinal Detachment?
Your retina can detach for several reasons, and it’s not always linked to trauma. The most common type of retinal detachment is rhegmatogenous detachment.
It occurs from a retinal tear, often linked to aging, trauma, or severe nearsightedness (myopia). On the other hand, tractional detachment causes the retina to pull away due to conditions like diabetic retinopathy.
Lastly, fluid can leak beneath the retina due to inflammation or tumors, detaching the retina. This is known as exudative detachment, and it can be associated with age-related macular degeneration (AMD), trauma, tumors in the eye, and inflammatory conditions.
What are the Risk Factors of Retinal Detachment?
Retinal detachment is relatively rare, affecting approximately 1 in 10,000 people per year. However, several factors can increase your risk of retinal detachment, including:
- Age. People 50 or older are at a higher risk of retinal detachment.
- High myopia. Greater than -6.0 diopters significantly raises your chances.
- Previous eye surgery. Especially cataract removal, which slightly elevates risk.
- Genetics. A family history of retinal detachment can increase your risk of retinal detachment.
- Trauma or injury. Sudden impacts can cause retinal tears and lead to detachment, which may occur immediately or days to weeks later.
- Eye diseases. Conditions like uveitis, lattice degeneration, and retinoschisis can result in retinal detachment.
- Diabetes. Diabetes can lead to diabetic retinopathy, which damages the retina’s blood vessels, causing scar tissue to form on the retina.
Is Retinal Detachment Serious?
A detached retina is a medical emergency that requires immediate care. Fortunately, early detection and treatment can protect your vision.
Here’s what you need to watch out for:
- Flashes of light. These appear as brief sparks or lightning streaks, especially in dim lighting. These can appear in one or both eyes (photopsia).
- Eye floaters. You might see specks, lines, or cobweb shapes floating in your vision.
- Vision loss. A dark shadow or curtain that blocks your peripheral (side) vision, often progressing towards the center.
Retinal cells cannot get the nourishment and oxygen needed from blood vessels when detachment occurs. Left untreated, retinal detachment can worsen and lead to permanent vision loss.
How is Retinal Detachment Diagnosed?
A doctor must diagnose and treat retinal detachment. If the examination reveals no holes or tearing despite your symptoms, your doctor will schedule a follow-up visit.
Tests used to diagnose detachment include:
- Dilated eye exam. Involves placing special eye drops to widen your pupils. They’ll then examine the back of your eye with a bright light.
- Ultrasound. If bleeding in the eye makes it difficult to examine the retina, your doctor might order an ultrasound to get a better view of the back of the eye.
You can also perform a quick self-check at home by covering one eye at a time. If your vision differs significantly between eyes or if you notice symptoms, seek immediate medical attention.
How is Retinal Detachment Treated?
A medical professional must treat retinal detachment, which requires surgery to correct. This is the only way to reattach the retina to receive the blood supply needed to remain healthy.
Your ophthalmologist will recommend the best approach based on your specific situation:
- Pneumatic retinopexy. A minimally invasive procedure that injects a small gas bubble into your eye, pressing the retina back into place. Ideal for small, upper retinal tears.
- Scleral buckle. A silicone band is secured around the eye, gently indenting the eye wall to reattach larger or more complex retinal detachments.
- Pars plana vitrectomy. Vitrectomy is often used for complex cases and involves a tiny incision to remove the vitreous gel (eye fluid), allowing surgeons to repair tears directly using laser therapy or cryotherapy.ne oil to fill the vitreous space and flatten the retina. The injected material is eventually absorbed, and the space refills with fluid.

These treatment methods have an 80% to 90% success rate. Additionally, newer techniques, such as 27-gauge vitrectomy and heads-up 3D visualization, are increasingly used and show outcomes comparable to standard approaches.
Each method requires anesthesia (often local) and typically between 30 minutes and 2 hours. Post-surgery, you'll need careful monitoring for complications like elevated intraocular pressure, cataracts, or recurrence.
What to Do After Treatment
Post-treatment care doesn’t end once your retina is reattached. Preventing further vision loss requires ongoing vigilance and routine check-ups:
- Regular follow-ups. Most surgeons examine you on postoperative day 1, then again around 1 week and 1 month; later visits are individualized to detect complications or recurrence early.
- Monitoring risks. Your other eye faces a higher chance of detachment. Your doctor may recommend prophylactic laser treatment if lattice degeneration or early tears appear, though its routine use remains debated.
- Managing chronic risks. Managing conditions like diabetes reduces the risk of vision-threatening diabetic retinopathy (and thus tractional detachments).
- Protective eyewear. Use protective eyewear during sports or high-risk activities to prevent injury.
How to Prevent Retinal Detachment
There is no guaranteed way to prevent retinal detachment. However, there are some things you can do to reduce your risk, including:
- Get regular eye exams to monitor your nearsightedness.
- Use protective eyewear when playing sports or working in hazardous environments.
- Seek medical attention as soon as possible if you experience symptoms.
In this article







