Updated on April 29, 2025
Lacrimal Gland Anatomy and Functions


Vision Center is funded by our readers. We may earn commissions if you purchase something via one of our links.
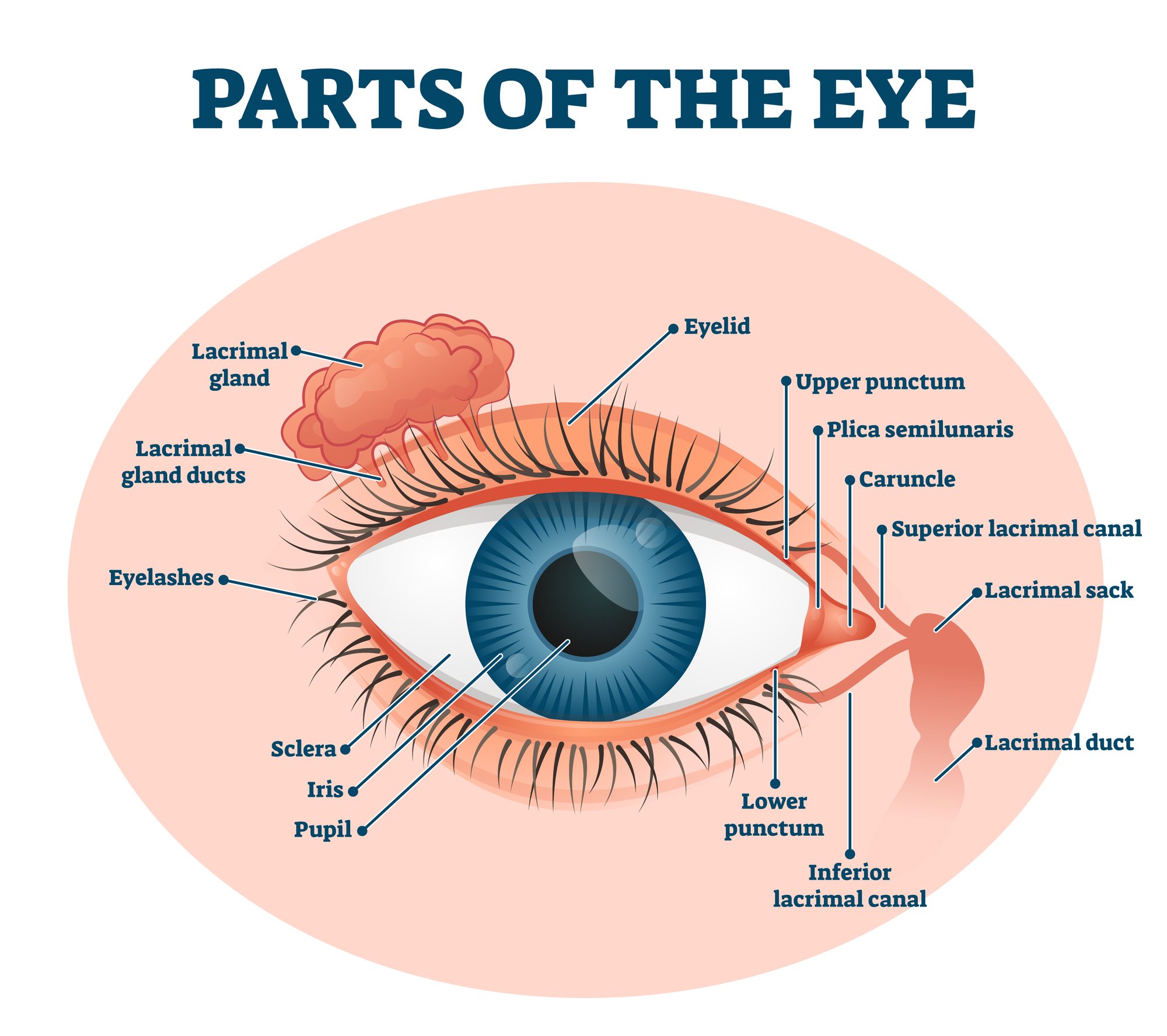
The lacrimal gland is a small organ in the human eye that secretes the watery portion of the tear film (lacrimal fluid).
These help clean, lubricate, nourish, and maintain eye health.1 When secreted in high amounts, it results in excessive tearing.
Anatomy and Functions of the Lacrimal Gland
Both eyes have one lacrimal gland measuring about 2 cm long. The lacrimal gland is one of the structures responsible for tear production.
Lacrimal Gland Components
The lacrimal gland is made up of two parts:
- Orbital lobe. Larger and located along the sideward margin of the muscle that maintains the upper eyelids’ position (levator palpebrae superioris muscle)
- Palpebral lobe. Smaller and located on the inner surface of the eyelid
Drainage and Fluid Distribution

The eye’s lacrimal gland has about 12 main drainage ducts. These ducts extend from the outer part of the gland, passing through a thin tissue called the levator palpebrae superioris aponeurosis.
The ducts open at the superior conjunctival fornix, the protective covering that allows lid and eye globe movement. From here, the ducts can release the fluid into the eye surface.2 Blinking helps spread the fluid on the eye surface.
This is how tear fluid circulates within the eye:
- As tear fluid moves in the eye, it gathers in a small pool called the "lacrimal lake" near the inner corner of the eye.
- From there, the tears flow into something called the "lacrimal sac." The lacrimal sac is located in the inside corner of your eye. It acts like a reservoir that stores the tears until they're ready to be released.
- Finally, your tears go down a duct system into the nose called the nasolacrimal duct system .
Accessory Lacrimal Glands
In addition to the main lacrimal gland, accessory lacrimal glands such as the glands of Krause and Wolfring also exist.3 They're much smaller than the lacrimal gland but similar in structure.
Accessory lacrimal glands account for about 10% of the total lacrimal secretion. The upper eyelid has more accessory lacrimal glands than the lower eyelid.
Where is the Lacrimal Gland Located?
The lacrimal gland is located above the eyeball towards the upper outer corner of the eye socket. It’s near other eye structures, including:
- Lacrimal nerve. An ophthalmic nerve
- Lacrimal artery. A branch of the ophthalmic artery
Related Conditions and Treatments of the Lacrimal Gland
The conditions affecting the lacrimal gland often result from inflammation. They include:
1. Dacryoadenitis
Dacryoadenitis refers to the inflammation of the lacrimal gland.4 The inflammation can be acute or chronic and affect one or both eyes.
Acute dacryoadenitis is more common among children and young adults.5 Chronic dacryoadenitis is rare.
Research shows that the condition is more common among females than males. This is because females are at a higher risk of systemic autoimmune diseases.
Symptoms include:
- Eye pain/tenderness
- Red eyes
- Droopy eyelid
- Problems opening eyes
- Excess tearing
- Swollen lymph nodes in front of the ear
- Blurred or double vision
Causes
Acute dacryoadenitis is caused by viruses, bacteria, and fungi (rare). Chronic dacryoadenitis results from noninfectious inflammatory disorders such as:
- Sarcoidosis
- Thyroid eye disease
- Sjogren syndrome
- Wegener's granulomatosis
- Orbital pseudotumor
Sometimes, dacryoadenitis can be idiopathic, meaning it has no known cause.
Treatment
Treatment for dacryoadenitis will depend on the cause and severity of the condition. It might include:
- Symptomatic treatment such as warm compress for viral dacryoadenitis such as mumps
- Systemic broad-spectrum antibiotics for bacterial dacryoadenitis
- Surgical drainage, in the case of abscess formation
- Oral corticosteroids for idiopathic dacryoadenitis
- Orbital radiation or systemic therapy for refractory cases
2. Chalazion
A chalazion is a swollen lump on an eyelid. It usually results from clogged meibomian glands.
Meibomian glands are located in the waterline of the upper and lower eyelids. These glands lining the eyelid margin produce oil that prevents tears from drying out.
Symptoms include:
- A painless lump (usually on the upper eyelid)6
- A firm lump
- Teary eyes
- Mild eye irritation
- Blurred vision in the case of a large chalazion
Causes
The meibomian glands produce oil that mixes with tears to keep the eye moist. When the oil is too thick, it can clog up the passage. Accumulated oil in the clogged gland leads to chalazion formation.
Some underlying inflammatory conditions might also cause chalazia. These include:
- Diabetes
- Stye infection
- Seborrheic dermatitis
- Acne rosacea
- Viral infections
- Meibomian gland dysfunction
Treatment
A chalazion usually goes away on its own. However, some home remedies can help manage the healing process.
These remedies include:
- Warm compress. Hold a damp and warm washcloth over the affected eye for about 15 minutes, three times daily, to unblock the oil gland.
- Gentle massages. Massaging the eyelids can open up the clogged glands.
- Good hygiene. Keeping your eyes clean and avoiding makeup can improve the healing process.
If a chalazion persists, your eye doctor might recommend fluid drainage through a small incision. They might also inject steroids to reduce swelling and inflammation.
Doctors do not recommend squeezing or popping it, as this can cause eye injury.
3. Watery Eyes (epiphora)
Epiphora is a condition where excess tears flow out of the eyes and down the face for no apparent reason. This condition can develop at any age, but it's most common among children under 12 and adults over 60.7 Epiphora can affect one or both eyes.
Symptoms include:
- Excess tears in the eye
- Blurry vision due to excess tears
- Tears involuntarily draining down your face
- Red eyes
- Soreness
- Eye pain
- Eyelid swelling
- Light sensitivity
Causes
In most cases, watery eyes result from an overproduction of the lacrimal fluid or poor drainage due to blocked tear ducts. Other causes include:
- Exposure to allergens or chemicals
- Eye infections
- Eye trauma (injury)
- Poorly positioned eyelids
- A foreign object in the eye
- Dry eyes syndrome
Treatment
Most people with watery eyes recover without treatment. The best type of treatment will depend on the cause. Options include:
- Medications. Your eye doctor might prescribe antibiotics if your watery eye is due to an infection. They might also prescribe lubricating eye drops or artificial tears for dry eye irritation.
- Foreign object removal. Your doctor can remove a foreign object that is causing discomfort.
- Saline solution. This solution is used to unblock the tear duct. Your doctor might also use a probe to open the tear duct.
- Surgery. This is recommended in cases of severe blockage of tear ducts.
- Eyelid repair. Sagging eyelids (entropion or ectropion) can be restored to prevent abnormal positioning.
4. Dry Eyes
Dry eyes result from low levels of lacrimal fluid (tears) in the eyes. This causes a lack of lubrication when blinking, which can be uncomfortable.
According to research, one in five adults has dry eyes. This condition is more common among older people.8 It affects more females than males.
Symptoms include:
- Red eyes
- Stinging or burning sensations
- Light sensitivity
- Watery eyes
- Mucus near the eye
- Blurry vision
Causes
Dry eyes result from low tear production, poor drainage, or poor-quality tears. Other factors can also affect the rate of tear production or drainage.
These factors include:
- Age
- Gender
- Medical conditions (e.g. blepharitis)
- Medications (e.g. decongestants and antidepressants)
- Environmental conditions (wind, smoke, or dry weather can increase tear evaporation rate)
Tears are made up of oil, water, and mucus layers. Dry eye symptoms can develop if the three layers are dysfunctional or evaporate too quickly. Other causes include:
- Long-term use of contact lenses
- Refractive eye surgery such as LASIK
Treatment
Dry eyes can be chronic. Treatments are available to keep dry eyes comfortable and healthy.
Options include:
- Artificial tears. Addresses mild cases of dryness
- Tear conservation. Achieved by blocking the drainage ducts using tiny but removable silicone or gel-like plugs
- Cyclosporine eye drops. Stimulates more tear production
- Treating eyelid or ocular surface inflammation. Using prescription eye drops, warm compresses, eyelid cleaners, or ointments
5. Ocular Sarcoidosis
Sarcoidosis can affect any body part and is one of the leading causes of inflammatory eye disease. Systemic (or whole-body) sarcoidosis is more likely to affect the eye. When parts of the eye, such as the lacrimal gland, are affected, it's called ocular sarcoidosis.9
This condition may cause several eyelid abnormalities, including:
- Uveitis
- Orbital inflammation
- Episcleritis
- Conjunctival granuloma
- Optic neuropathy
- Lacrimal gland enlargement
Other symptoms include:
- Blurry vision
- Eye pain
- Severe red eyes
- Burning, itching, or dry eyes
- Sensitivity to light (photophobia)
Causes
The cause of ocular sarcoidosis is unknown. Some experts, however, associate it with an abnormal immune response.10
Studies have also linked it to infectious agents, certain chemicals, and environmental allergens. Others have linked it to genetics, meaning parents can pass it on to their children.11
Treatment
There's no cure for ocular sarcoidosis. However, various therapies can manage the condition. They include:12
- Corticosteroid therapy. Topical, oral, or intravenous corticosteroids are the first line of treatment
- Systemic immunosuppressive agents. Used instead of corticosteroids when prolonged steroid treatment is required (e.g., methotrexate and mycophenolate mofetil)13
- Biologic agents. Recommended when corticosteroids and immunosuppressive therapy fail
- Surgery. Cataracts and glaucoma are complications of ocular sarcoidosis; surgery involves the removal of media opacity, such as cataracts, which can affect vision
Summary
- The lacrimal gland, a small organ in the human eye, is located above the eyeball towards the upper outer corner of the eye socket.
- This gland secretes the watery part of tears (lacrimal fluid) that cleanses, lubricates, and nourishes the eyes, often causing tearing when produced excessively.
- The gland is divided into the larger orbital lobe and the smaller palpebral lobe.
- Conditions associated with the lacrimal gland encompass dacryoadenitis, chalazion, watery eyes, dry eyes, and ocular sarcoidosis.
- Diagnosis and suitable treatment recommendations are offered by eye doctors based on the specific cause and severity of the condition.
In this article
12 sources cited
Updated on April 29, 2025
Updated on April 29, 2025
About Our Contributors
Vincent Ayaga is a medical researcher and seasoned content writer with a bachelor's degree in Medical Microbiology. Specializing in disease investigation, prevention, and control, Vincent is dedicated to raising awareness about visual problems and the latest evidence-based solutions in ophthalmology. He strongly believes in the transformative power of ophthalmic education through research to inform and educate those seeking knowledge in eye health.
Dr. Melody Huang is an optometrist and freelance health writer with a passion for educating people about eye health. With her unique blend of clinical expertise and writing skills, Dr. Huang seeks to guide individuals towards healthier and happier lives. Her interests extend to Eastern medicine and integrative healthcare approaches. Outside of work, she enjoys exploring new skincare products, experimenting with food recipes, and spending time with her adopted cats.

