Updated on October 23, 2024
What Are Eye Floaters and Are They Dangerous?


Vision Center is funded by our readers. We may earn commissions if you purchase something via one of our links.
Eye Floaters, Spots, and Flashes: Overview
Eye floaters are spots you might see in your field of vision. They appear as gray or black specks, cobwebs, or strings that float around when your eyes move. If you try to look at them directly, they will dart away quickly.
Some spots can move around, while other floaters appear stationary. Other people may see flashes of light instead of spots, as if someone is turning the light switch on and off.

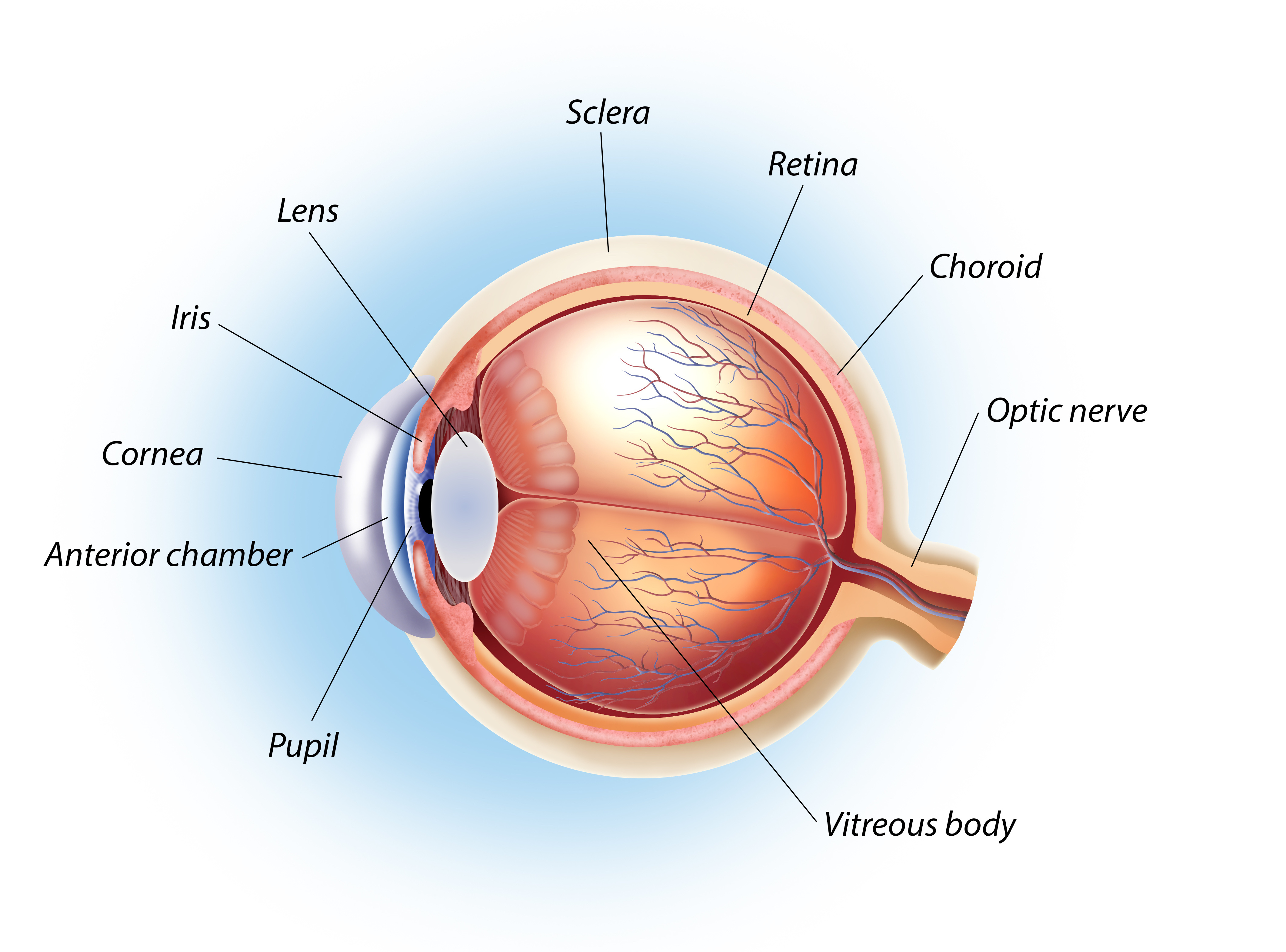
These symptoms occur from changes in the vitreous. Eye floaters are usually nothing but an annoyance. They are common and usually harmless.
However, if they impair your vision, make an eye exam appointment with your ophthalmologist. Worsening eye floaters or developing new floaters could be connected to an underlying condition.
Listen In Q&A Format
What are Eye Floaters?
Vision Center Podcast
Common Symptoms of Eye Floaters
Eye floaters can take on many forms. Some of these different shapes include:
- Cobwebs
- Black, grey, or translucent dots
- Worm-like strands
- Ring or partial ring
- Shadow in the vision
- Blurry spot in the vision
You may notice the floaters more when looking at a white background or a blue sky. Most people find floaters annoying, but they rarely interfere with vision unless the floater is large or dense.
Some people also see light flashes if the vitreous tugs on the retina. This symptom often occurs when the vitreous first starts to loosen and detach itself. This may or may not cause further complications.
6 Causes of Eye Floaters
Common factors contributing to eye floaters include: aging, eye infection, bleeding in the eye, cataract surgery, eye medication, and myopia (nearsightedness).
1. Aging
The vitreous changes properties as you age. It liquefies and compresses with time, causing it to pull away from the inside of the eyeball. These clumps are not entirely transparent and cast shadows on your retina. The shadows are what you see as floaters.
2. Eye infection
Eye infections can cause eye swelling and inflammation. For instance, uveitis, an inflammation of the eye's middle layer, can result in floaters. This is because cells can be kicked off into the vitreous when inflamed.
3. Bleeding in the Eye
Eye injuries or diseases like diabetic retinopathy can cause bleeding eyes. They can also cause retinal tears and detachment.
When these happen, the blood from the retina can get into the vitreous. This can cause spots and streaks in your vision.
4. Cataract Surgery
A cataract forms in the eye lens, which sits adjacent to your vitreous. Cataract surgery can disrupt your vitreous and retina.
The ultrasound waves used to break up the cataract during surgery increase your chances of floaters.
5. Eye Medication
In some cases, medications that are injected into the eye can result in air bubbles. These air bubbles look like shadows and can appear in your vision. They move around in your eye and appear as floaters.
6. Myopia (nearsightedness)
Nearsighted people typically have longer eyeballs. This elongation puts stress on your retina as the tissue thins and stretches outs. This stretching can also cause the vitreous attachments to loosen, increasing the risk for floaters.
Potential Risks of Eye Floaters
Floaters are typically harmless and don’t signal vision loss.
In rare cases, they can also be a sign of vision-threatening complications. Make an appointment with your ophthalmologist if your eye floaters worsen over several months.
Some eye diseases and conditions associated with floaters include:
Posterior vitreous detachment (PVD)
This common condition occurs when the back portion of the vitreous detaches completely from the retina.
Most posterior vitreous detachments do not cause any problems. However, if the vitreous only detaches partially, the vitreous can still pull on the retina.
You can develop a vitreous hemorrhage, retinal tear, or retinal detachment when this happens.
Retinal holes or tears
A retinal hole or tear can occur if the vitreous pulls on the retina with enough tension. Nearsighted people are more prone to these problems because they have thinner retinas.
Depending on the hole or tear size, your eye doctor can determine if treatment is necessary.
Retinal detachment
If fluid seeps into a retinal hole or tear, the fluid can start to build up underneath the retina. This can cause the tissue to detach.
A retinal detachment requires immediate medical attention. This is a vision-threatening condition.
The sooner a retinal detachment is repaired, the better the prognosis.
Vitreous hemorrhage
Several eye conditions can cause blood to leak into your vitreous. Some of these include:
- Diabetic retinopathy
- Retinal tears
- Posterior vitreous detachments
- Hypertensive (high blood pressure-related) retinopathy.
Patients with a vitreous hemorrhage may report floaters and often see blurry or red spots in their vision.
Migraines
Migraine symptoms are often confused with eye floater symptoms.
While migraines do not cause floaters, some people notice light flashes or see spots in their vision when a migraine occurs. These visual symptoms can also occur without a headache. This condition is called an ocular migraine.
Other causes of eye floaters include:
- Uveitis (inflammation of the middle of the eye)
- Hemorrhaging
- Eye injury
- Torn retina
When to see a doctor
See your eye doctor right away if you have the following: Symptoms of light flashes, A sudden increase in floaters, Shadows in your vision, A curtain over your vision.
- Symptoms of light flashes
- A sudden increase in floaters
- Shadows in your vision
- A curtain over your vision
These can be signs of a detached retina or retinal tear.
Eye Floaters Diagnosis
Your doctor will perform a complete eye exam to check for eye floaters. A dilated eye exam will also help your doctor get a clearer look inside your eye and retina.
During a dilated eye exam, your doctor will use eye drops to widen your pupils. This helps them check for eye floaters. The exam also allows your doctor to look for any signs of retinal tear.
Once you're diagnosed with eye floaters, your eye doctor will recommend treatment options based on your symptoms. Follow-up visits are important to track how well the treatments work.
You may be able to manage or reduce eye floaters naturally.
2 Treatment Options for Eye Floaters
Most eye doctors recommend not treating floaters unless they significantly interfere with your vision. If your floaters are very bothersome, treatment options are available to get rid of your floaters. Here are some of them:
1. Laser Vitreolysis
Laser vitreolysis is a less invasive way to remove floaters. This procedure is best for patients who have trouble with their floaters for 6 months or longer. If your floaters are relatively new, your eye doctor may recommend you monitor them.
What to Expect
During the procedure, the eye surgeon:
- Instills numbing drops into your eye
- Places a special magnifying contact lens onto your eye
- Targets a laser to dissolve your floaters
Potential Risks
As with any medical procedure, there are potential risks. These risks include:
- Elevated eye pressure (higher risk of glaucoma)
- Cataracts
- Retinal tears
- Retinal detachments
Most patients notice some improvement in their vision after treatment. However, some patients require multiple treatments. There is also a chance the treatment may not improve your symptoms.
2. Pars Plana Vitrectomy
Pars plana vitrectomy is a type of eye surgery that treats conditions in the retina or vitreous. These include retinal detachments or vitreous hemorrhages.
This surgery is more invasive than laser vitreolysis. Many eye doctors discourage having this procedure done if your floaters are not causing complications.
In cases of extreme floaters, a vitrectomy can remove them from your eye.
What to Expect
During a vitrectomy, the eye surgeon:
- Administers local anesthesia to numb your eye (they use general anesthesia in some patients)
- Makes a small incision in the white part of your eye called the sclera
- Inserts microsurgical tools through these incisions to remove your vitreous
- Replaces the vitreous with silicone oil or a gas bubble
Possible Risks
Risks of vitrectomy include:
- Elevated eye pressure (higher risk of glaucoma)
- Cataracts
- Infection
- Swelling in the retina
- Retinal tears
- Retinal detachments
In this article
7 sources cited
Updated on October 23, 2024
Updated on October 23, 2024
About Our Contributors
Alyssa is a content contributor and lead editor for Vision Center. She has a Master's degree in Journalism and over 6 years of professional experience writing expert-backed content in the health/medical space, including eye care and vision health. Her goal is to provide up-to-date information that is easy to understand, medically accurate, and engaging.
Dr. Melody Huang is an optometrist and freelance health writer with a passion for educating people about eye health. With her unique blend of clinical expertise and writing skills, Dr. Huang seeks to guide individuals towards healthier and happier lives. Her interests extend to Eastern medicine and integrative healthcare approaches. Outside of work, she enjoys exploring new skincare products, experimenting with food recipes, and spending time with her adopted cats.

