Updated on October 10, 2024
The Anatomy and Function of the Sclera

Vision Center is funded by our readers. We may earn commissions if you purchase something via one of our links.
What is the Sclera?
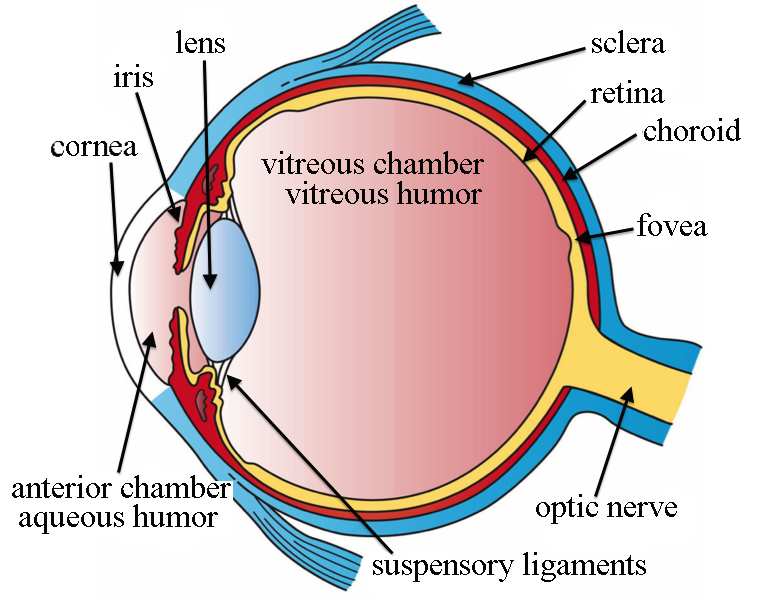
The sclera is commonly known as the white of the eye. It’s the opaque tissue that surrounds your entire eyeball, except for the clear cornea (the covering in the front of your eye).
The sclera is strong, fibrous tissue made mostly of collagen and elastic fibers.
What is the Anatomy of the Sclera?
Scleral tissue forms more than 80 percent of the surface area of the eyeball. It’s made of durable collagen fibers extending from the cornea in front of the eye to the optic nerve in the back.
The sclera contains many nerves and blood vessels that enter through the optic nerve canal.
Four layers comprise the human sclera. These include (in order from outermost to innermost layer):
- Episclera
- Stroma
- Lamina fusca
- Endothelium
The bulbar conjunctiva covers the front part of your sclera. This is a thin layer of tissue with blood vessels.
What Is the Function of the Sclera?
The sclera’s dense connective tissue forms the supporting wall of the human eyeball and gives it its white color.
The sclera and intraocular pressure maintain the shape and structural integrity of the eyeball. It also protects the inner structures of your eye from trauma.
Most of your eyeball is filled with a gel-like fluid called the vitreous humor. Your extraocular muscles, which control your eye movements, attach firmly to the sclera.

Sclera Problems
Several conditions can affect the sclera. Some problems appear to affect the sclera but actually affect the overlying bulbar conjunctiva. The appearance can be misleading because the bulbar conjunctiva is mostly transparent.
Sclera conditions include:
Episcleritis
Episcleritis is an inflammation of the outermost layer of the sclera. Symptoms include:
- Redness
- Mild pain
- Swelling of the conjunctiva
- Eyelid swelling
- Raised nodules on the eye
Most cases are sectoral, meaning only a section of the sclera is affected. In diffuse cases, the entire sclera can be affected. Episcleritis may be associated with rheumatoid arthritis, lupus, Crohn’s disease, Behcet’s disease, or gout.
Scleritis
Scleritis is inflammation of the sclera. It can be similar to episcleritis, but more serious and painful. Scleritis often causes intense pain that worsens with eye movement. It can be caused by an injury or underlying inflammatory condition.
If left untreated, this condition is more severe than episcleritis and may cause permanent damage and vision loss.
Scleromalacia Perforans
Scleromalacia perforans is a rare and severe condition. Your immune system attacks the sclera tissue, causing significant thinning and bulging.
Because of thinning, the underlying uveal tissue is visible. This gives the sclera a bluish appearance. In rare cases, the eye can rupture. Scleromalacia perforans is often associated with older women with long-standing rheumatoid arthritis.
Scleral Icterus (Jaundice)
Scleral icterus is jaundice that affects the eyes. It gives the whites of the eyes a yellow appearance. The name is not entirely accurate because it affects the conjunctiva, not the sclera. It is sometimes known as conjunctival icterus.
This condition occurs when your body has high bilirubin levels. Bilirubin is a yellowish substance that is produced from the breakdown of red blood cells. Liver disease or other serious health conditions can cause high bilirubin levels.
Scleral Plaques
Scleral plaques are blue-gray calcified plaques that appear on the sclera. They are related to old age. They are benign and do not cause any symptoms.
Blue Sclera
Blue sclera occurs when the sclera thins, exposing the dark, uveal tissue underneath (where it gets its blue color).
The cause may be congenital (present at birth). Osteogenesis imperfecta (brittle bone disease) can cause it. Blue sclera is also associated with Marfan syndrome, Ehlers-Danlos syndrome, and Loeys-Dietz syndrome.
Acquired blue sclera may be a sign of severe iron deficiency.
Types of Congenital Scleral Abnormalities
Other conditions present at birth that may affect the sclera. Some of these are harmless. Others are more severe and may affect vision or eye health.
Ocular Melanosis
Ocular melanosis is pigmentation of the conjunctiva overlying the sclera. They typically look like flat, brown spots on the white part of the eye, similar to a freckle on the skin. Melanosis can be congenital or acquired.
There are two acquired forms, primary and secondary acquired melanosis:
- Primary acquired melanosis. Is more common in light-skinned individuals and may grow in size. In rare cases, it may develop into malignant (cancerous) melanoma.
- Secondary acquired melanosis. Is associated with hormonal changes, radiation exposure, chemical exposure, or metabolic disorders. People with darker skin and hair are more likely to have it. This form rarely develops into melanomas.
Nevus of Ota (Oculodermal Melanocytosis)
Nevus of Ota is a congenital condition. It causes hyperpigmentation of the eye, eyelids, and other surrounding areas. The pigment often appears blue or brown.
Typically, the nevus doesn’t require treatment. Some people desire laser therapy to lighten the spots for cosmetic reasons. Nevus of Ota is associated with a higher risk of glaucoma and, in rare cases, eye melanoma.
Ectasia (Staphyloma)
Ectasia is a congenital thinning and bulging of the sclera.
The thinning usually occurs near the limbus and also affects the cornea. The staphyloma often presents with a blue appearance.
Staphylomas can also develop on the back of the eye, particularly in people with high myopia (nearsightedness).
Scleral Coloboma
Colobomas occur when there is some tissue missing in the eye at birth. This results in the incomplete formation of a particular structure of the eye.
Colobomas can affect the eyelid, iris, lens, optic nerve, choroid, and retina. The optic nerve, choroidal, or retinal colobomas can cause scleral thinning and staphylomas.
When to Call a Healthcare Professional
Contact your healthcare provider if you notice any changes to your vision or the appearance of your sclera.
Concerning signs and symptoms to look out for include:
- Discoloration of the sclera
- Blurry vision
- Sensitivity to light
- Pain or tenderness
- Eyeball swelling or bulging
Types of Sclera Procedures & Surgeries
The following procedures treat problems with the sclera:
Scleral Expansion
Scleral expansion is a somewhat controversial procedure designed to treat presbyopia.4 Presbyopia is the loss of the ability to focus up close with age.
The surgery involves inserting four plastic pieces into the sclera between the eye muscles. This technology is still improving, and some researchers feel this procedure could become the gold standard in presbyopia treatment.
Scleral Buckle
A scleral buckle procedure is performed to repair a retinal detachment.
During the surgery, a doctor uses cryopexy (freezing therapy) to seal your retina to the eye. Then they’ll place a silicone or plastic band around your eyeball (the scleral buckle). This helps the retina stay in place, and the buckle is permanent.
Summary
The sclera is known as the white of the eye. It helps maintain your eye shape and protects your inner structures from eye trauma.
Different problems may affect the sclera, there are procedures and surgeries available to manage them. If you experience any symptoms of these problems, consult your doctor immediately.
In this article
8 sources cited
Updated on October 10, 2024
Updated on October 10, 2024
About Our Contributors
Dr. Melody Huang is an optometrist and freelance health writer with a passion for educating people about eye health. With her unique blend of clinical expertise and writing skills, Dr. Huang seeks to guide individuals towards healthier and happier lives. Her interests extend to Eastern medicine and integrative healthcare approaches. Outside of work, she enjoys exploring new skincare products, experimenting with food recipes, and spending time with her adopted cats.
