Updated on October 1, 2024
What Are Corneal Ulcers?

Vision Center is funded by our readers. We may earn commissions if you purchase something via one of our links.
What is a Corneal Ulcer?
A corneal ulcer is an open sore or wound on the cornea, known as the transparent outer layer of your eye. The cornea is responsible for maintaining clear vision.
Eye infection is the leading cause of corneal ulcer. A minor corneal injury, or even contact lens complications, can bring on such an infection.
Infections that may lead to a corneal ulcer include:
- Bacterial keratitis
- Fungal keratitis
- Acanthamoeba keratitis
- Herpes simplex keratitis
How Serious Is an Ulcer in the Eye?
A corneal ulcer is a medical emergency that requires prompt treatment. Untreated corneal ulcers or eye infections can lead to severe vision loss, scars, or the loss of an eye.
Contact your eye doctor right away if you develop eye pain or other symptoms of a corneal ulcer.
What Are The Symptoms of a Corneal Ulcer?
Most corneal ulcers are quite painful. Your cornea has the highest concentration of nerve fibers compared to any other part of your body. This makes it incredibly sensitive, which is why ulcers cause so much pain.
Symptoms of corneal ulcers include:
- Significant eye pain
- Light sensitivity
- Inability to keep eyes open from pain and light sensitivity
- Redness of the eye
- Foreign body sensation (feels like sand or eyelash in the eye)
- Tearing
- Blurry vision
- Soreness of the eye
- Swollen eyelids
- Discharge
- Visible white spot on the cornea
At first, corneal ulcer symptoms may resemble those of pink eye (conjunctivitis).
How Is a Corneal Ulcer Diagnosed?
Your eye doctor can diagnose your corneal ulcer by examining your eyes under a microscope called a slit-lamp.
They may instill a yellow dye called fluorescein into your eye. Then, your doctor will view your eye with a special blue light.
If there’s a corneal ulcer, the dye will highlight the affected area. The ulcer will appear to glow under the blue light.
Seek treatment immediately. Untreated corneal ulcers can lead to corneal scarring, blindness, or the loss of your eye.
How Is a Corneal Ulcer Treated?
Treatment for a corneal ulcer focuses on treating the underlying cause. This typically involves taking medicine to fight the specific type of infection.
Medications may come in the form of eye drops or oral pills. They include:
- Antibiotic drops (for bacterial infections)
- Antiviral drops or oral medications (for viral infections)
- Antifungal drops or oral medications (for fungal infections)
If you’re experiencing severe eye pain, your eye doctor may prescribe drops that dilate your pupils. These eye drops may provide pain relief while your eyes are inflamed. In some cases, your eye doctor may add a steroid eye drop to decrease the chances of corneal scarring.
With corneal ulcers, most eye doctors will follow you closely over several days or even weeks, depending on the severity of the ulcer. These visits are essential to see if your condition is improving.
Should You Wear Contact Lenses or an Eye Patch for a Corneal Ulcer?
You shouldn’t wear contact lenses or use an eye patch while you have a corneal ulcer. Covering the affected eye doesn’t promote healing. However, you should wear protective glasses to keep dust and debris out of your eye.
You should also avoid wearing eye makeup until the healing process is complete.
When Is Surgical Treatment Needed for a Corneal Ulcer?
Severe ulcers and those that don’t resolve with medications may require corneal transplant surgery. A corneal transplant involves surgically removing the infected corneal tissue and replacing it with donor tissue.
Like any surgical procedure, a corneal transplant involves certain risks. Potential complications include:
What Causes a Corneal Ulcer?
There are infectious and non-infectious (sterile) corneal ulcers. Most ulcers come from bacterial infections, but there are several other causes as well.
Bacterial Infections
These are the most common type of infectious corneal ulcers, especially in contact lens users.
Contact lenses can trap bacteria, allowing the bacteria to multiply. People who sleep in their contacts, use dirty contacts, or reuse old contacts have a higher risk of infectious ulcers.
Viral Infections
Corneal ulcers can result from a viral infection of:
- Herpes simplex. The same virus that causes cold sores on the lips. Herpes simplex keratitis can be triggered by stress, sunlight, or a suppressed immune system.
- Herpes zoster. The same virus that causes chickenpox and shingles.
Fungal Infections
These infections are less common than those caused by bacteria. They’re more likely to occur in humid areas where mold and yeast can multiply.
Most people with fungal keratitis have been exposed to plants, such as someone who works in landscaping.
Parasitic Infections
Acanthamoeba is a type of amoeba that lives in freshwater. Acanthamoeba keratitis occurs when this amoeba infects your eye.
This type of infection is rare but severe and extremely painful. Some risk factors for Acanthamoeba infection include using contaminated tap water or swimming in ponds or other bodies of freshwater.
Non-Infectious Corneal Ulcers
Aside from infections, other causes of corneal ulcers include:
Severe Allergic Eye Disease
Certain types of eye allergies, called atopic or vernal keratoconjunctivitis, can cause corneal ulcers.
Atopic keratoconjunctivitis usually affects older adults, while vernal keratoconjunctivitis typically affects younger males. These types of eye allergies are rare.
Corneal Abrasions
A corneal abrasion is a scratch or cut on the surface of the eye. If a corneal abrasion gets infected by bacteria, it can lead to a corneal ulcer.
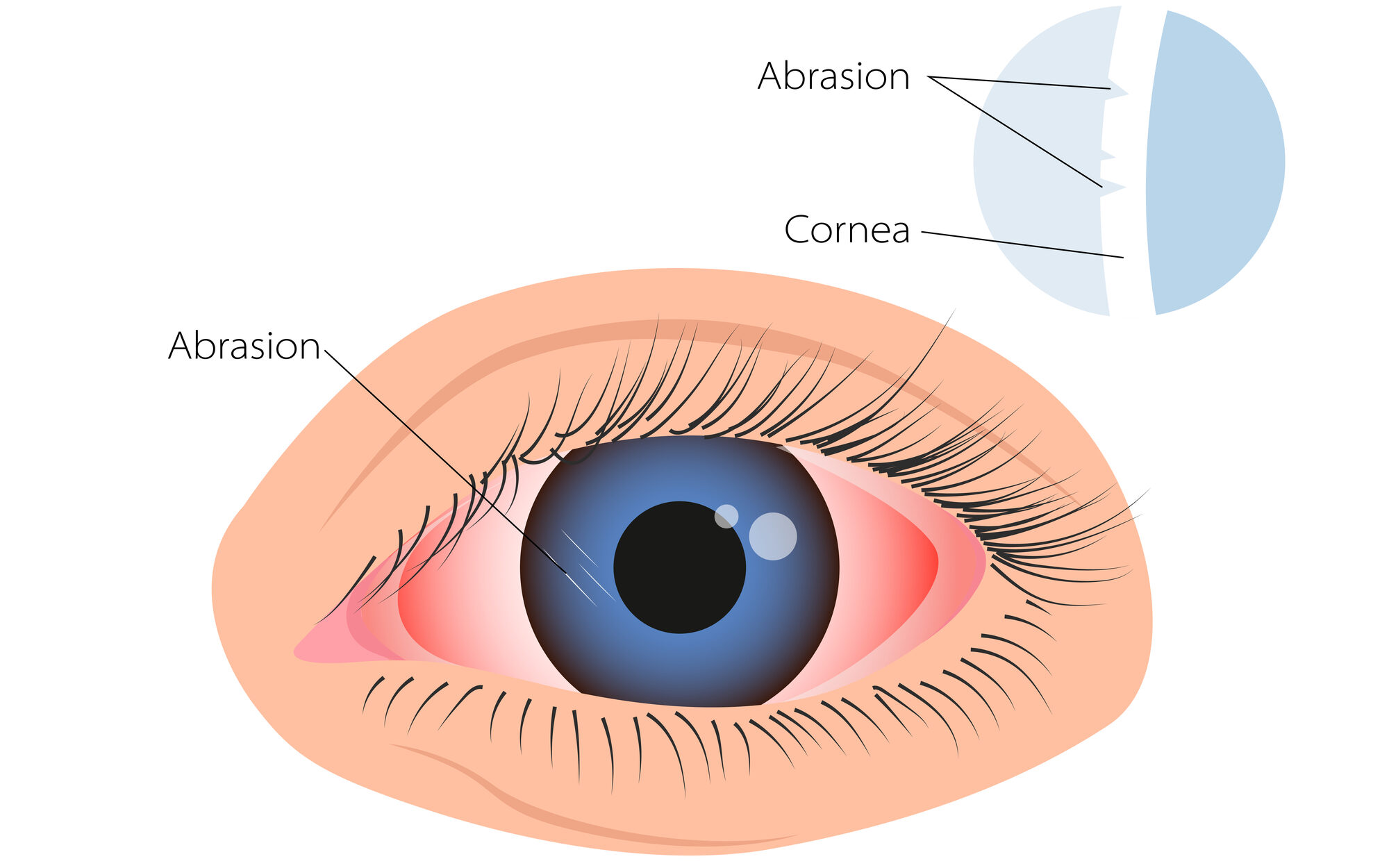
Common causes of corneal abrasions include:
- Scratches from fingernails or other sharp objects
- Chemical burns
- Particles of dirt trapped in the eye
Improper Use of Contact Lenses
Contact lens wearers are at higher risk for corneal ulcers. Wearing contact lenses may lead to an eye infection or corneal ulcer if you:
- Wear soft contacts that have expired
- Wear disposable contacts longer than recommended
- Sleep while wearing contact lenses
- Don’t properly clean, disinfect, and store your contact lenses
Other Causes
Other conditions that may cause corneal ulcers include:
- Severe dry eye
- Eye injury
- Vitamin A deficiency
- Autoimmune diseases
- Inflammatory disorders
Are Corneal Ulcers Preventable?
Protecting your eyes and maintaining good eye hygiene can help reduce your risk for corneal ulcers. Here are some general tips for preventing corneal ulcers, particularly infectious types:
- Wash your hands before touching your eyes
- Clean your contact lenses properly, and always use fresh solution and a clean case
- Don’t sleep in contact lenses or use them longer than directed
- Only use contact lens solution to clean and store lenses — never water or saliva
- Remove all eye makeup before sleep and discard old makeup
- Wear eye protection around dust, dirt, or other particles that can enter your eyes
- Use lubricating eye drops to moisturize your eyes
Summary
A corneal ulcer is an open wound on the cornea. The cornea is the clear dome at the front of your eye that provides sharp vision. A corneal ulcer is a medical emergency that can result in vision loss.
Most corneal ulcers are caused by infections, but they can result from other causes as well. Treatment focuses on treating the underlying cause of the corneal ulcer.
A corneal ulcer is a serious eye problem that can lead to permanent vision loss. When diagnosed and treated early, most people recover from a corneal ulcer. However, the ulcer may cause permanent scarring on the eye that can affect vision.
In this article
6 sources cited
Updated on October 1, 2024
Updated on October 1, 2024
About Our Contributors
Dr. Melody Huang is an optometrist and freelance health writer with a passion for educating people about eye health. With her unique blend of clinical expertise and writing skills, Dr. Huang seeks to guide individuals towards healthier and happier lives. Her interests extend to Eastern medicine and integrative healthcare approaches. Outside of work, she enjoys exploring new skincare products, experimenting with food recipes, and spending time with her adopted cats.
