Eye allergies affect millions of individuals each year, causing itching, redness, and discomfort that can disrupt daily life.
Recent data suggests the prevalence of allergic conjunctivitis (the medical term for eye allergy) may be on the rise, influenced by factors such as climate shifts, changing allergen exposures, and increased urbanization.
This article explores the core statistics surrounding eye allergies to understand the scale and impacts of this common yet often under-recognized condition. We’ll examine prevalence rates, demographic breakdowns, economic costs, and preventive measures, offering a data-driven view of how eye allergies shape public health and quality of life.
Key Statistics at a Glance
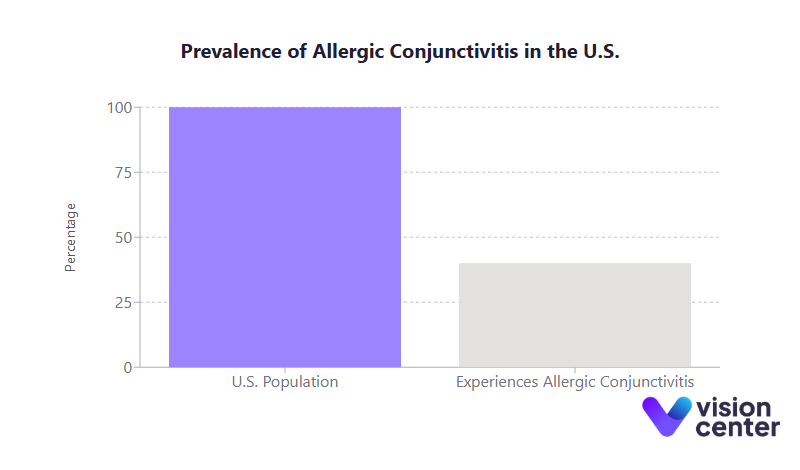
- Up to 40% of the U.S. population experiences some form of allergic conjunctivitis.
- Among children worldwide, as many as 30% have been found to develop eye allergy symptoms.
- Seasonal pollen peaks can lengthen by 2 to 3 weeks in certain regions, intensifying and prolonging seasonal eye allergies.
- Eye allergies, coupled with other allergic conditions like allergic rhinitis, contribute to billions of dollars in direct and indirect costs annually in the United States.
Understanding the Scope of Eye Allergies
Eye allergies, often referred to as allergic conjunctivitis, occur when the tissues lining the eyelids and covering the whites of the eyes (the conjunctiva) react to allergens. This reaction leads to itching, redness, tearing, and swelling, symptoms that, while typically not vision-threatening, can severely hamper day-to-day activities.
Over the last decade, statistics indicate that allergic conjunctivitis remains one of the most common ocular conditions in both adults and children. The data also shows that, in many cases, eye allergies are accompanied by nasal allergies or other atopic conditions (like asthma or eczema), reflecting an overarching pattern of interconnected allergic diseases.
Why These Data Matter
Examining the numerical trends in eye allergy prevalence helps clinicians, policymakers, and patients identify who is most at risk and when symptoms are most likely to strike. These figures also highlight the broader societal impact both in terms of productivity and financial costs. By recognizing the scale of eye allergies and their frequent comorbidities, stakeholders can design interventions that better address prevention, treatment, and long-term management.
- High Prevalence Across Age Groups
- Approximately 25 to 30% of adults report seasonal allergies that include eye symptoms.
- An estimated 20% or more of children suffer from seasonal allergies, with ocular involvement in most cases.
- Seasonal vs. Perennial Allergies
- Seasonal triggers (pollen from grasses, trees, weeds) cause spikes in allergic conjunctivitis, notably in spring and fall.
- Perennial triggers (dust mites, pet dander, indoor molds) result in year-round symptoms that may flare intermittently.
- Regional Variation
- Warmer, humid regions (particularly in the Southern U.S.) report some of the highest eye allergy rates.
- Northern states are seeing longer pollen seasons, intensifying and extending the typical windows for seasonal allergic conjunctivitis.
Demographic Breakdowns and Trends
Why Demographics Are Important
Demographic data shed light on which population groups are most susceptible to eye allergies. Understanding patterns by age, gender, and race/ethnicity can help tailor public health campaigns and clinical approaches. It also underscores potential genetic or environmental factors that might explain why certain individuals or communities have higher eye allergy risks.
- Gender Differences
- In children, boys often exhibit higher seasonal allergy rates than girls (close to a 2 to 3% difference).
- In adulthood, women generally report more frequent or severe seasonal allergy symptoms than men, with some surveys showing about 30% of women and 21% of men affected.
- Childhood Onset
- Many people develop allergies in childhood or adolescence.
- Severe allergic conjunctivitis subtypes (e.g., vernal keratoconjunctivitis) often manifest first in younger patients and can persist into early adulthood.
- Elderly Populations
- Adults aged 65+ do experience allergic conjunctivitis, though slightly lower rates are reported (sometimes below 25%).
- Immune system changes and reduced outdoor exposure may explain the lower prevalence among older adults.
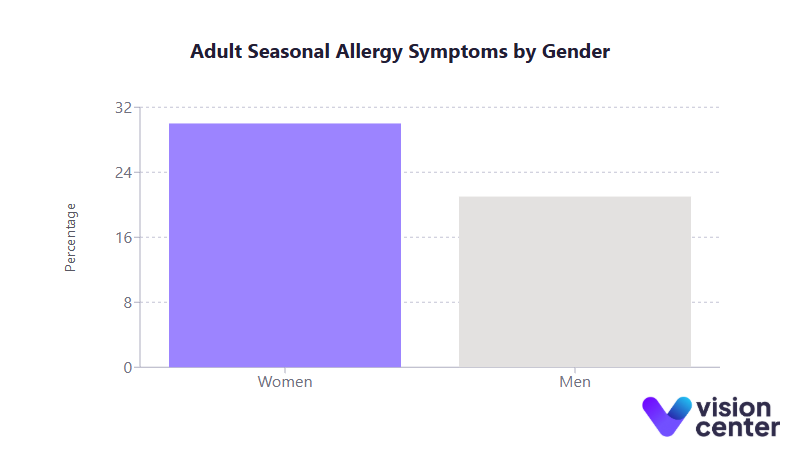
Table: Approximate Eye Allergy Prevalence by Age Group
| Age Group | Estimated Seasonal Allergy Rates (Including Eye Symptoms) |
| Children (0–17) | ~19% (though global estimates for ocular allergies in children can approach 30%) |
| Adults (18–64) | 25 to 30% |
| Seniors (65+) | ~20 to 25% |
Economic Burden and Quality of Life Impacts
Why Costs and Quality of Life Data Are Crucial
Eye allergies can seem minor compared to more severe illnesses. Yet, they account for substantial direct costs (doctor visits, medications, tests) and indirect costs (missed work or school, reduced productivity). Additionally, the persistent discomfort (itchy, watery eyes) can affect concentration, reading ability, computer use, and overall well-being.
- Productivity Loss
- Allergies (including ocular symptoms) contribute to an estimated 4 million missed workdays per year in the United States.
- “Presenteeism” is also common; many individuals show up to work but struggle to perform at full capacity.
- Direct Medical Costs
- Across the United States, the annual direct costs for allergic rhinitis (often paired with eye symptoms) are in the $3 to 4 billion range.
- Over-the-counter (OTC) products for eye allergy relief account for a significant share of patient out-of-pocket spending.
- Quality of Life Burdens
- More than 50% of individuals with environmental allergies (including eye allergies) say symptoms interfere with daily activities.
- Children with untreated or severe allergic conjunctivitis can experience setbacks in school performance and social participation due to persistent irritation and lack of focus.
Seasonal Patterns and Environmental Factors
Why Seasonal Tracking Matters
Knowing when eye allergies peak each year can guide both individual preventive care and public health planning. In spring, tree and grass pollens surge, often triggering intense ocular symptoms. Late summer into fall sees weed pollen (e.g., ragweed) dominating, creating a second peak.
- Rising Pollen Counts
- Climate shifts are lengthening pollen seasons in many northern U.S. regions; some areas have seen a 2 to 3 week extension of the ragweed pollen season over recent decades.
- Hot, dry, and windy days disperse pollen widely, exacerbating symptoms; rainy weather often lowers pollen count and reduces eye irritation.
- Perennial Triggers
- Indoor allergens, such as dust mites and pet dander, cause year-round conjunctivitis symptoms, though they can spike during higher humidity seasons.
- Mold spores flourish in damp environments, often creating flare-ups in rainy or poorly ventilated indoor spaces.
Treatment Effectiveness and Outcomes
Why Treatment Data Is Important
Eye allergy management has evolved with new, more effective medications and a better understanding of preventive approaches. Data-driven insights show which therapies provide the fastest relief and how well they maintain symptom control.
- Rapid Symptom Relief
- Modern antihistamine/mast-cell stabilizer eye drops take effect within minutes and can offer relief for 8 to 12 hours.
- Single-dose, once-daily formulations (e.g., certain olopatadine strengths) let many patients remain symptom-free through most of the day.
- Long-Term Management
- Consistent use of mast cell stabilizer drops before and throughout allergy season prevents severe flare-ups.
- In chronic or severe cases, short-term topical steroid drops or immunomodulators (like cyclosporine) may be needed, under close medical supervision.
- High Efficacy Rates
- Clinical trials show that most patients on topical antihistamine regimens experience a marked drop in itchiness, redness, and tearing within 5 to 10 minutes.
- Proper adherence (i.e., using drops as recommended daily) significantly boosts quality of life and reduces the likelihood of eye rubbing and subsequent complications.
Prevention Strategies and Future Outlook
Why Prevention Data Matters
Because eye allergies are driven by environmental triggers (pollen, pet dander, dust mites) prevention often starts with avoidance measures and seasonal planning. Over time, immunotherapy can offer more lasting relief by reducing overall sensitivity.
- Allergen Avoidance
- Keeping windows closed, relying on air conditioning, and showering after outdoor activities are all proven strategies to reduce pollen exposure.
- For dust mite or pet dander allergies, measures like mite-proof bedding covers and vacuuming with HEPA filters can greatly lower indoor allergen levels.
- Immunotherapy (Desensitization)
- Allergen-specific immunotherapy (via shots or sublingual tablets) can deliver 70 to 80% success rates in reducing ocular and nasal allergy symptoms long term.
- Extended courses of 3 to 5 years often lead to fewer prescriptions needed and milder seasonal flare-ups afterward.
- Planning Ahead
- Starting eye drop regimens (especially mast cell stabilizers) 1 to 2 weeks before pollen season can prevent or lessen the severity of allergic conjunctivitis.
- Checking daily pollen counts allows individuals to schedule outdoor activities for lower-risk times and take extra precautions on high-count days.
Final Thoughts
Eye allergy statistics reveal a condition that is both widespread and deeply influential on daily life. In recent years, more people have reported symptoms triggered by pollen, dust, pets, and mold, driven partly by environmental shifts and prolonged allergen seasons.
The demographic data shows that eye allergies can affect individuals at all stages of life, with varying rates by gender, age, and region. Meanwhile, the economic costs underscore that these issues extend beyond mere itching or redness.
Ultimately, the data encourages a balanced, informed view: while eye allergies remain common and can be disruptive, consistent management and preventive efforts can markedly reduce their impact. In addressing this prevalent condition, both individual actions and wider public health initiatives can work hand in hand.
By aligning strategies with the growing body of statistical research, we can continue to refine our understanding of eye allergies and help millions find relief for years to come. Moving forward, leveraging data-driven insights will remain crucial to guiding improved treatments, reducing healthcare costs, and enhancing quality of life for those affected by this ubiquitous condition.
In this article


