Age-related vision loss has become an increasingly urgent concern, especially as medical advances allow people to live longer. While many older adults maintain healthy eyesight, a significant portion experience progressive conditions that gradually diminish their vision and independence.
Although routine eye exams and modern treatments have reduced blindness rates for several conditions, the total number of individuals with age-related vision loss continues to climb. Below is a data-driven look at the scope and impact of these disorders, along with trends in prevention and treatment and the burden on patients and caregivers alike.
Overview of Age-Related Vision Loss
Vision loss in the elderly often stems from four major conditions: age-related macular degeneration (AMD), glaucoma, diabetic retinopathy, and cataracts. Each of these diseases can develop silently, sometimes displaying few symptoms until significant damage has already occurred.
Together, they rank among the top causes of visual impairment and blindness in individuals over 60. Crucially, modern therapies are now helping many older adults preserve or restore their vision. Even so, the growing number of seniors has translated into a sharp rise in the overall prevalence of age-related eye conditions in the United States over the past 20 years.
Beyond its clinical aspects, age-related vision loss carries broad social and economic consequences. Older adults with vision impairment often experience declines in quality of life, ranging from limitations in daily tasks to increased rates of loneliness and depression.
Likewise, caregivers supporting visually impaired seniors bear a substantial load, dedicating extra time to help with activities that sighted individuals perform routinely. As America’s population ages, these challenges will continue to shape healthcare policies and resource allocation in the years ahead.
Key Statistics at a Glance
- By 2050, the total number of Americans with uncorrectable vision impairment (partial sight or blindness) is projected to more than double, surpassing 8 million people.
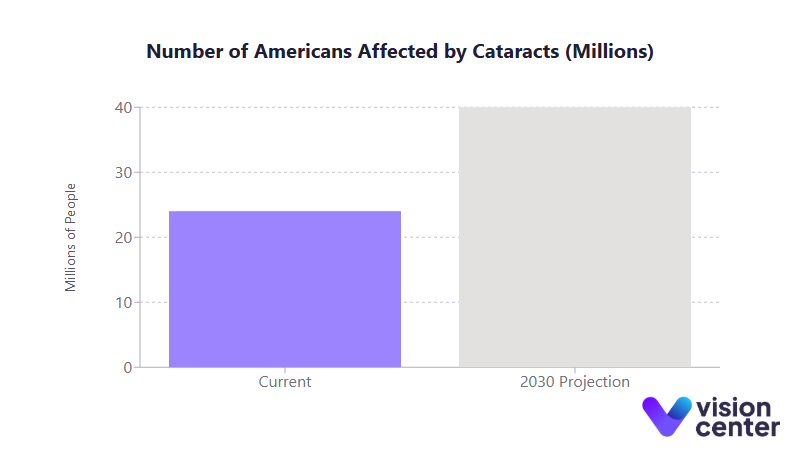
- Cataracts currently affect over 24 million Americans; this figure is expected to reach nearly 40 million by 2030.
- An estimated 2.1 million Americans had advanced AMD in 2010, a number that may exceed 5 million by 2050.
- Annual economic costs attributable to vision loss in the U.S. are estimated at over $130 billion, factoring in both direct medical expenses and indirect social burdens.
Prevalence and Demographics
Understanding how common age-related vision loss is and which groups are most at risk forms the starting point for addressing this public health challenge. Accurate prevalence data help shape screening guidelines, allocate healthcare resources, and highlight at-risk populations requiring proactive interventions.
- Age as a Key Factor
- Close to half of Americans aged 85 and older have some form of AMD, whereas under 2% of adults in their early 40s are affected.
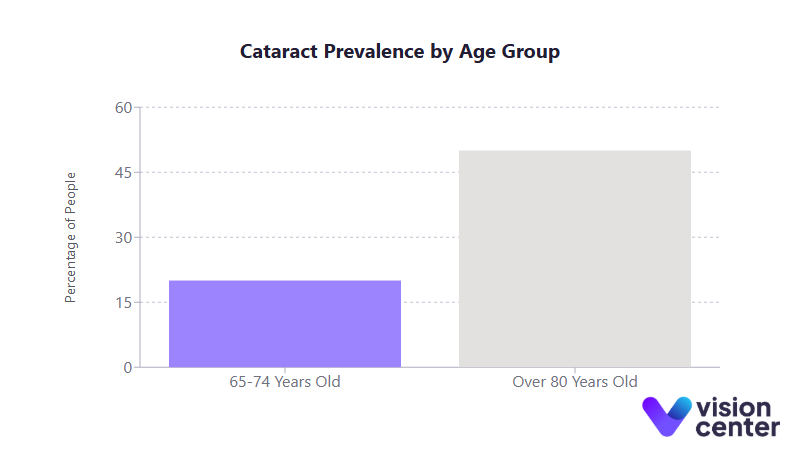
- For cataracts, about 20% of people aged 65 to 74 report significant lens clouding or vision impairment; that figure climbs above 50% in those over 80.
- Condition-Specific Numbers
- AMD: Approximately 2.1 million had advanced AMD in 2010. The total with any form of AMD (including early stages) is still growing, currently estimated at nearly 20 million in adults over 40.
- Glaucoma: More than 2.7 million Americans over 40 have this optic nerve disorder, and glaucoma prevalence is expected to double by 2050.
- Diabetic Retinopathy: About 9.6 million people with diabetes in the U.S. have some degree of retinopathy, with nearly 2 million at immediate risk of vision-threatening complications.
- Cataracts: At least 24 million individuals experience cataracts, with age being the most significant contributor to lens degeneration.
- Geographic and Racial Disparities
- States with a higher average age, such as Florida, often have AMD prevalence exceeding 15% among adults over 40, compared to less than 7% in the District of Columbia.
- In regions where diabetes rates are high (particularly in portions of the Southern United States), diabetic retinopathy affects larger segments of the population.
- Glaucoma is 3 to 4 times more prevalent among Black Americans than White Americans, contributing to racial disparities in blindness rates.
Below is a simplified table illustrating select estimates of major eye conditions among U.S. adults aged 40 and older:
| Condition | Estimated Prevalence (Current) | Projected Prevalence (Future) |
| AMD (Any Form) | ~20 million | 30+ million by mid-century (all stages) |
| Advanced (Wet) AMD | 2.1 million in 2010 | 5+ million by 2050 |
| Glaucoma | 2.7+ million | ~6.3 million by 2050 |
| Diabetic Retinopathy | ~9.6 million (26% of diabetics) | Rising due to increased diabetes rates |
| Cataracts | ~24 million | 38 to 40 million by 2030 |
Key Influencing Factors
Recognizing why some populations develop age-related vision loss faster or more severely than others is essential for strategic interventions. Many of these diseases result from a complex mix of genetics, lifestyle factors, and access to healthcare.
- Lifestyle and Systemic Health
- Smoking significantly elevates the risk for AMD and cataracts.
- Poor blood sugar control accelerates diabetic retinopathy; tight glycemic management lowers progression rates.
- Cardiovascular factors (such as hypertension and high cholesterol) have also been linked to faster progression of AMD and some forms of retinopathy.
- Socioeconomic Status and Healthcare Access
- Regular eye screenings help detect diseases like glaucoma and early diabetic retinopathy before vision loss occurs, but screening rates can be low in underserved areas.
- Patients in rural or economically disadvantaged regions often face greater barriers to care, resulting in later diagnoses and more advanced disease at first presentation.
Trends Over Time (2005 to 2025)
Over the past two decades, the aging Baby Boomer generation has contributed to a marked rise in cases of macular degeneration, glaucoma, diabetic retinopathy, and cataracts.
Even when prevalence rates (i.e., percentages) for some conditions have stabilized or decreased modestly, the sheer number of older adults means the total pool of individuals with vision impairment keeps expanding.
- Between 2005 and 2025, the number of older adults with cataracts and glaucoma grew significantly, and projections show a continued upward climb through mid-century.
- AMD incidence per age group dropped somewhat, attributed to healthier diets, better cardiovascular care, and reduced smoking. Still, the total number of people with AMD is growing.
- Diabetic retinopathy prevalence is steadily rising as diabetes itself becomes more common. Recent estimates suggest almost 10 million Americans with diabetes now have some level of retinal changes.
As a result, uncorrectable vision impairment is on track to reach or exceed 8 million affected individuals by 2050, underscoring the need for robust public health planning and expanded access to ophthalmic care.
Intervention Effectiveness
Data show that while these eye conditions often pose significant threats to vision, early detection and modern treatments can substantially improve outcomes.
- Prevention and Early Detection
- Tight control of blood sugar and blood pressure substantially reduces the onset and progression of diabetic retinopathy.
- Smoking cessation lowers AMD risk, and high-dose antioxidant supplements (commonly referred to as the AREDS formula) can slow the progression of intermediate AMD by about 25%.
- Regular screenings for glaucoma, particularly among older adults and high-risk groups, are vital because the disease often remains asymptomatic until substantial vision damage has occurred.
- Treatment Advances
- AMD (Wet Form): Anti-VEGF injections can stabilize vision in around 90% of patients and, in many cases, even improve sight. This marks a dramatic improvement over older therapies that had limited benefits in halting rapid vision loss.
- Glaucoma: By lowering eye pressure via medications, laser therapy, or surgery, the risk of disease progression and blindness can be cut by roughly half. Modern techniques have reduced the probability of going blind in at least one eye by up to half compared to rates from two decades ago.
- Diabetic Retinopathy: Laser photocoagulation slashes the risk of severe vision loss by more than 50% if applied before advanced complications. Anti-VEGF injections for diabetic macular edema further increase the chance of significant vision improvement.
- Cataract Surgery: Often hailed as one of the safest and most effective surgeries, cataract removal restores usable vision in 9 out of 10 patients, with minimal risk of severe complications.
Collectively, these interventions have transformed the prognosis of age-related eye disease. Patients diagnosed and treated in earlier stages now enjoy a higher likelihood of maintaining functional vision into advanced age.
Healthcare Utilization
A major factor in understanding age-related vision loss is how these conditions strain healthcare resources and generate costs.
- Economic Burden
- Annually, vision loss in the U.S. accounts for well over $130 billion in direct and indirect costs.
- Glaucoma alone generates around $5.8 billion each year, with per-patient treatment often exceeding $2,000 annually for medications, monitoring, and surgical interventions.
- Anti-VEGF treatments for AMD and diabetic macular edema can cost thousands of dollars per injection and frequently require repeated doses, raising total costs substantially.
- Long-term care expenses for seniors who lose their independence can be the biggest financial outlay of all. Many older adults with advanced vision loss require extensive home care or nursing home placement.
- Clinical and Rehabilitative Services
- Eye care visits, ranging from dilated exams to laser treatments and surgeries, have climbed steadily in the past two decades as the older population grows.
- Intravitreal injections for AMD and diabetic macular edema now number in the millions annually, reflecting the adoption of anti-VEGF as a standard of care.
- Cataract surgery rates have also grown, often surpassing 3 million procedures per year nationwide.
- Vision rehabilitation services, including training on assistive devices and mobility skills, remain underutilized, leaving many visually impaired seniors without the full spectrum of supportive care.
Impact on Patients and Caregivers
Statistical measures of prevalence, cost, and clinical efficacy only capture part of the story. At the human level, age-related vision loss can profoundly disrupt daily life and strain family relationships.
- Quality of Life for Older Adults
- Even mild vision deficits can limit driving, reading, medication management, and recognizing faces.
- Vision loss correlates strongly with increased rates of depression, heightened fall risk, and earlier admission into long-term care facilities.
- Surgical interventions (e.g., cataract removal) or low-vision aids can improve quality of life significantly, but many older adults still face isolation if their vision cannot be fully corrected.
- Caregiver Burden
- Family members providing assistance to seniors with poor eyesight often log 30% more hours of care compared to those supporting individuals without visual impairments.
- Tasks such as reading mail, paying bills, and organizing medications become daily responsibilities.
- The emotional load on caregivers can be considerable: elevated rates of anxiety and depression are commonly found in those caring for loved ones with severe vision loss.
By recognizing both the clinical and personal dimensions of the problem, policymakers, healthcare systems, and advocacy organizations can better target resources to limit the toll of age-related vision loss.
Final Summary
In recent years, the scope of age-related vision loss has expanded as the overall population ages, and the associated costs to both individuals and healthcare systems have grown in tandem.
Meanwhile, advances in treatments have collectively improved outcomes. Still, millions of Americans struggle with significant vision impairment, and not all have equal access to cutting-edge therapies.
By combining proven preventive measures with ongoing treatment innovation, experts hope to curb the worst outcomes and preserve the quality of life for an ever-growing population of older adults. Looking ahead, the upward trend in new cases underscores the importance of continued research, awareness, and policy development.
Ultimately, addressing age-related eye conditions is not just about preventing blindness, it’s about safeguarding independence, mobility, and mental well-being for millions of people in their later years. By prioritizing early detection, affordable eye care, and robust patient support services, the nation can take meaningful steps toward reducing the impact of age-related vision loss on individuals, families, and communities.
In this article


