Updated on October 1, 2024
How Does Diabetes Affect the Eyes and Vision?


Vision Center is funded by our readers. We may earn commissions if you purchase something via one of our links.
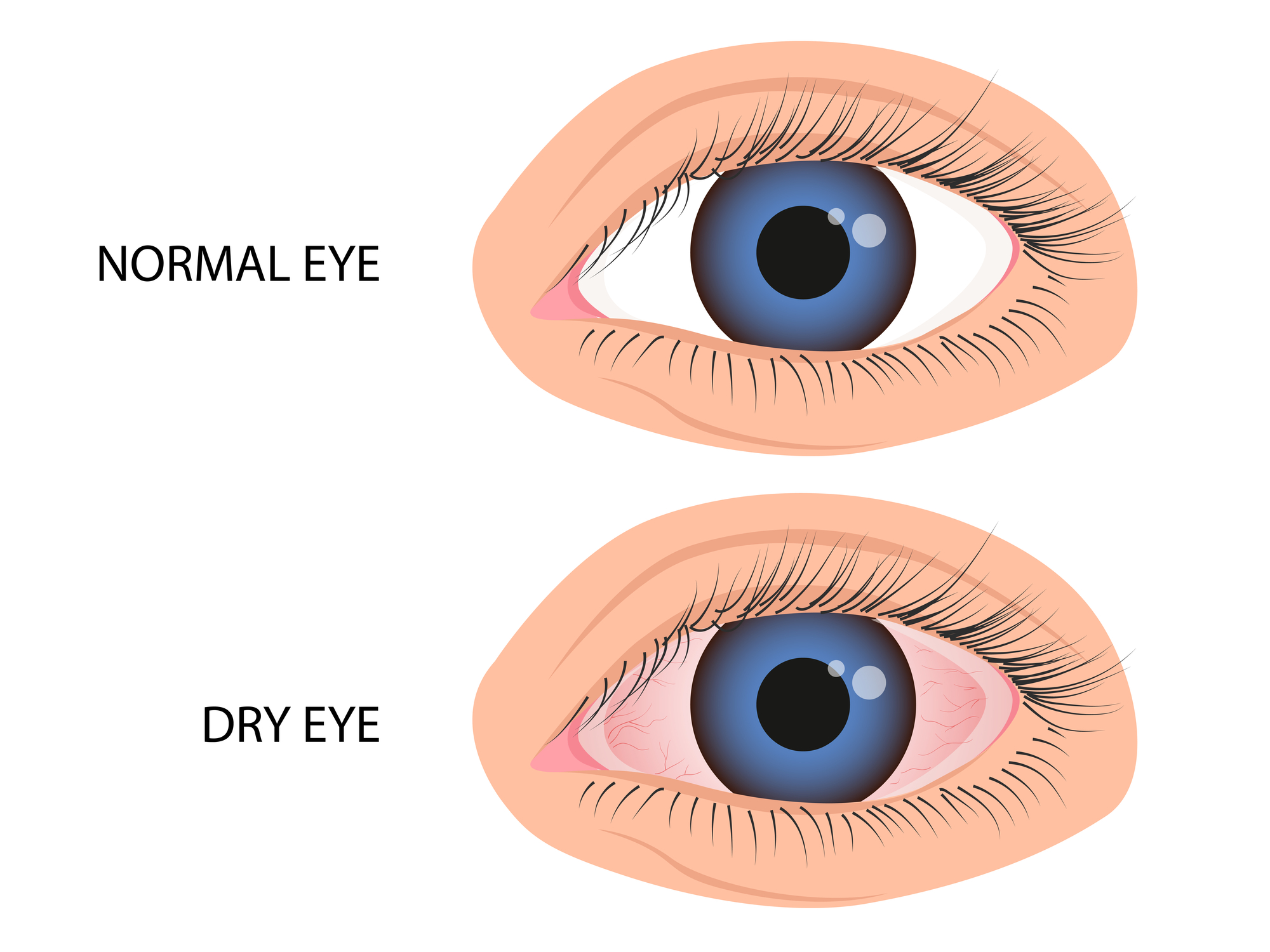
Dry eye syndrome affects millions worldwide. The condition primarily results from insufficient tear production and tear film dysfunction. Dry eyes can feel uncomfortable, and in some cases, vision issues may occur.1
The risk of developing dry eye disease increases if you:
- Have certain medical conditions such as lupus or Sjögren syndrome
- Take certain drugs like blood pressure medications
- Are female
- Are aged 50 or older
- Wear contact lenses
In this article, we look at diabetes and its connection to dry eyes.
Does Diabetes Cause Dry Eyes?
Dry eye syndrome is a common symptom of Type 1 and 2 diabetes. Recent studies indicate that about 53% of people with diabetes mellitus are at risk of dry eyes.2
Dry eyes are more common among those with Type 2 diabetes. The risk increases if the disease is more severe.
How to Manage Diabetes-Related Dry Eyes
Proper diabetes management is the best way to prevent diabetes-associated dry eyes. However, no significant differences exist between dry eye management and treatment for those with and without diabetes.
Below are effective treatment management strategies for diabetes-related dry eyes:
1. Artificial Tears
Using artificial tears creates a tear film that lubricates the eye and improves comfort. Healthcare professionals recommend using preservative-free artificial tears due to the risk of epithelial tissue damage associated with chemical preservatives such as benzalkonium chloride (BAK).6
2. Eye Gels and Ointments
If artificial tears aren’t enough, eye gels and ointments are denser, creating lasting effects. Apply the gel or ointment before bed and shut your eyes for at least 15 minutes. Avoid using the ointments during the day, as they can blur your vision.
3. Humidifier
Diabetics living in low-humid areas can benefit from a humidifier. A humidifier increases the moisture level in your space, reducing tear evaporation.
4. Warm compresses
Apply a warm damp cloth or pad on the dry eye for 10 minutes. The heat applied during a warm compress will improve oil gland function and increase oil flow into the eyes. It will stabilize the tear film and prevent drying.
5. Lifestyle Changes
You can relieve dry eye symptoms by implementing lifestyle changes such as:
- Eating a proper diet (rich in lutein, zeaxanthin, and vitamin C)
- Quitting smoking
- Taking breaks, especially after eye-straining activities such as extended screen time.
- Use disposable contact lenses to prevent the build-up of dirt and bacteria. Also, avoid sleeping in your eye contact lens to let your eyes breathe.
6. Blinking More Often
Frequent blinking helps keep the tear film intact for long. When your eyes are glued to a book or screen, you blink less, and the tears evaporate faster, leaving the eyes dry.7
How Does Diabetes Cause Dry Eyes?
People with diabetes don’t produce enough insulin to convert blood sugars into energy, causing high blood sugar levels.3 Too much sugar can damage blood vessels and nerves, including the lacrimal gland and cornea.
The lacrimal gland supports the tear film’s water production. When nerves in these glands are damaged, the quality and amount of tears are affected, causing dry eyes.
Effects of Diabetes on the Eyes
In addition to dry eyes, diabetes can affect the eyes in other ways:
1. Diabetic Corneal Neuropathy
The cornea is the transparent front layer of the eye. It’s the most densely innervated tissue in the human body.
Elevated blood glucose (hyperglycemia) damages the cornea’s nerves, resulting in diabetic corneal neuropathy. This condition also compromises the corneal epithelium, tear film, and stroma. It affects about 18% of patients with diabetes.4
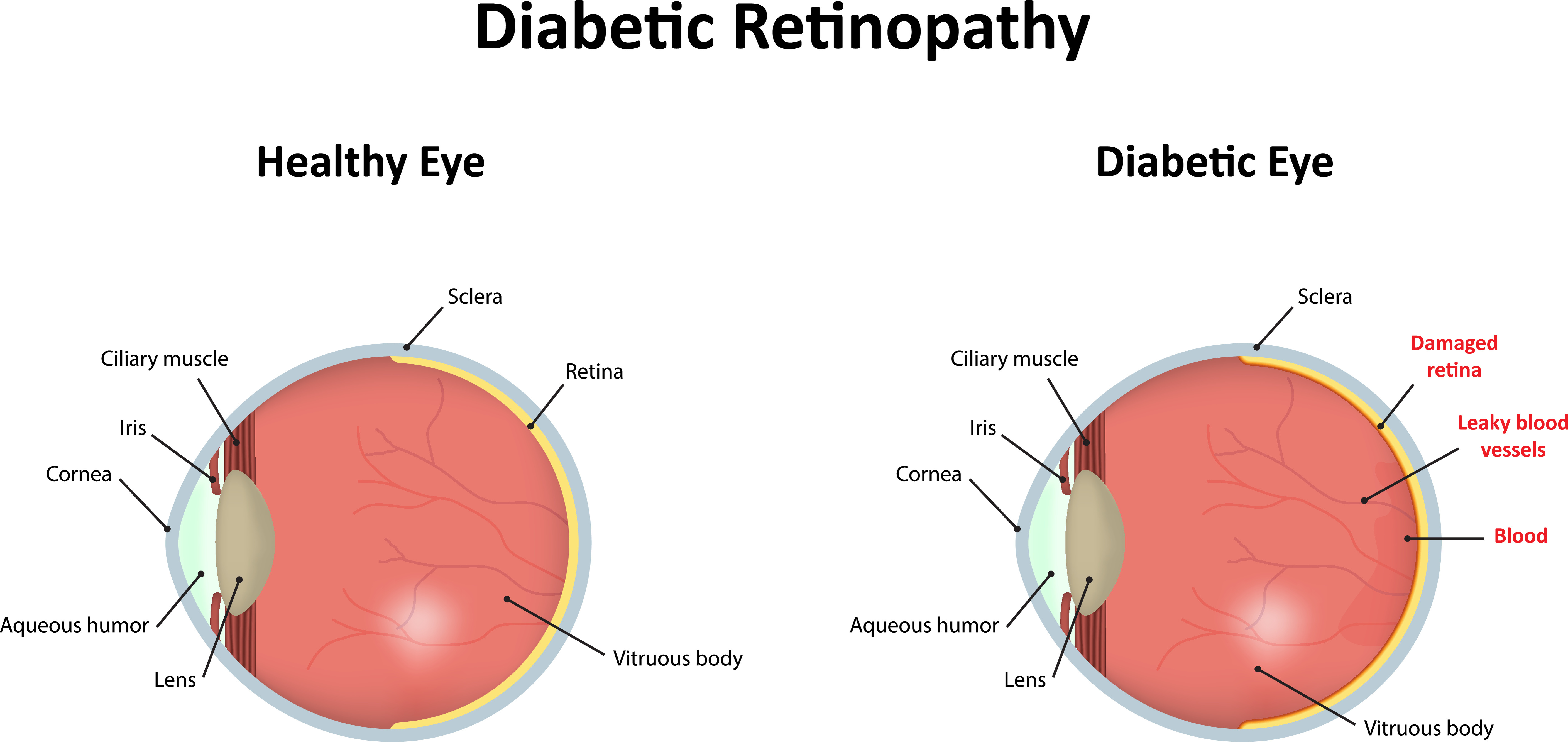
2. Diabetic Retinopathy
Diabetic retinopathy is a common complication of diabetes. It occurs when elevated blood glucose damages the blood vessels in the retina.
The retina is the light-sensitive layer at the back of your eye. The damaged vessels can swell and leak into the eye, causing vision problems, including permanent eye damage.
3. Blurry Vision
Elevated blood sugar levels can cause swelling and changes in eye lens shape. Your sugar levels may fluctuate, causing episodes of blurry vision.
4. Cataracts
A cataract is characterized by clouding the usually clear eye lens. Long-term high blood sugar can cause structural changes in the eye lens, accelerating the development of cataracts.
How Does Diabetic Retinopathy Affect Vision?
Diabetic retinopathy is known to cause vision issues, including blindness in severe cases.5 According to the Centers for Disease Control and Prevention (CDC), diabetic retinopathy has two main stages.
These are the two stages of diabetic retinopathy:
Early Stage (Nonproliferative)
The nonproliferative stage of diabetic retinopathy is the most common. The existing retinal blood vessels weaken, bulge, and leak into the retina.
When the retina swells, it’s called macular edema. Macular edema is a leading cause of blindness among diabetic patients.
You may not notice symptoms in early-stage diabetes. Healthcare professionals recommend a dilated eye exam at least once a year for early diagnosis and treatment.
Advanced Stage (Proliferative)
The proliferative stage of diabetic retinopathy is when the retina grows new abnormal blood vessels. These blood vessels often leak into the vitreous, the clear fluid that fills between the lens and the retina.
Abnormal blood vessels growing in the drainage angle cause glaucoma that may completely impair your vision. Clinical characteristics of diabetic retinopathy include:
- Floating spots
- Blurred vision
- Red eyes
- Eye pain
- Fluctuating vision
- Double vision (diplopia)
- Blindness
Treatment Strategies for Diabetic Dry Eyes
Below are common definitive treatment measures for diabetic dry eyes.
| Treatment Strategy | Effect |
| Managing blood sugar levels (insulin) | Prevents eye damage and keeps tear glands functioning correctly |
| Eye drop medications | Stimulates tear production |
| Punctal occlusion | Suppresses quick tear drainage |
| Prescription medications (cyclosporine and lifitegrast) | Help eyelid oil glands function normally |
| Autologous blood serum drops (AS) | Serum creates artificial tears to relieve dry eye symptoms8 |
| Nasolacrimal treatments | Eye drop alternatives like Tyrvaya (nasal spray) and iTear100 (neurostimulator device) stimulate tear production |
| Vitamin C and E supplements | Cause less oxidative stress and decreased nitric oxide levels, relieving dry eye symptoms9 |
| Dry eye glasses | Wrap and protect the eyes from elements such as dust, winds, and sunlight |
| Amniotic membrane | Rich in anti-inflammatories and growth hormones that stimulate ocular damage repair |
Can Diabetes Affect the Eyes Permanently?
Yes, diabetes can affect your eyes permanently if not well managed. In severe cases, like diabetic retinopathy, damaged vessels may leak into the macula (macula edema), causing vision loss. Retinal detachment due to scarring at the back of the eye can also cause vision loss.
If vision loss occurs, it will be too late to restore it. This is why regular eye exams are recommended to diagnose vision problems early and prevent them from worsening.
Summary
- Dry eye syndrome is a common symptom of diabetes Type 1 and Type 2 (53% of diabetics are at risk)
- Other ocular effects of diabetes include diabetic retinopathy, macula edema, blurry vision, cataracts, and glaucoma
- You may not notice symptoms in early-stage diabetes, necessitating a dilated eye exam at least once a year for early diagnosis and treatment
- Consult your healthcare provider if you suspect dry eye disease and other vision problems due to diabetes
- Diabetic dry eye treatment and management strategies include managing blood glucose levels, warm compresses, artificial tears, antibiotic eye drops, etc
In this article
10 sources cited
Updated on October 1, 2024
Updated on October 1, 2024
About Our Contributors
Vincent Ayaga is a medical researcher and seasoned content writer with a bachelor's degree in Medical Microbiology. Specializing in disease investigation, prevention, and control, Vincent is dedicated to raising awareness about visual problems and the latest evidence-based solutions in ophthalmology. He strongly believes in the transformative power of ophthalmic education through research to inform and educate those seeking knowledge in eye health.
Dr. Melody Huang is an optometrist and freelance health writer with a passion for educating people about eye health. With her unique blend of clinical expertise and writing skills, Dr. Huang seeks to guide individuals towards healthier and happier lives. Her interests extend to Eastern medicine and integrative healthcare approaches. Outside of work, she enjoys exploring new skincare products, experimenting with food recipes, and spending time with her adopted cats.

