Updated on February 20, 2024
How Does Diabetes Affect the Eyes?


Vision Center is funded by our readers. We may earn commissions if you purchase something via one of our links.
Diabetes is a common and serious disease affecting over 37 million people in the U.S., over 11% of the population.1 It’s a lifelong condition that causes high blood glucose (blood sugar) levels.
When blood sugar is too high, the entire body, including the eyes, is affected. Left unmanaged, diabetes can ravage eye health and cause serious vision problems. However, there are steps you can take to help prevent this from happening.
This article covers diabetic eye disease, including risk factors, prevention, and treatment.
How Does Diabetes Affect the Eyes?
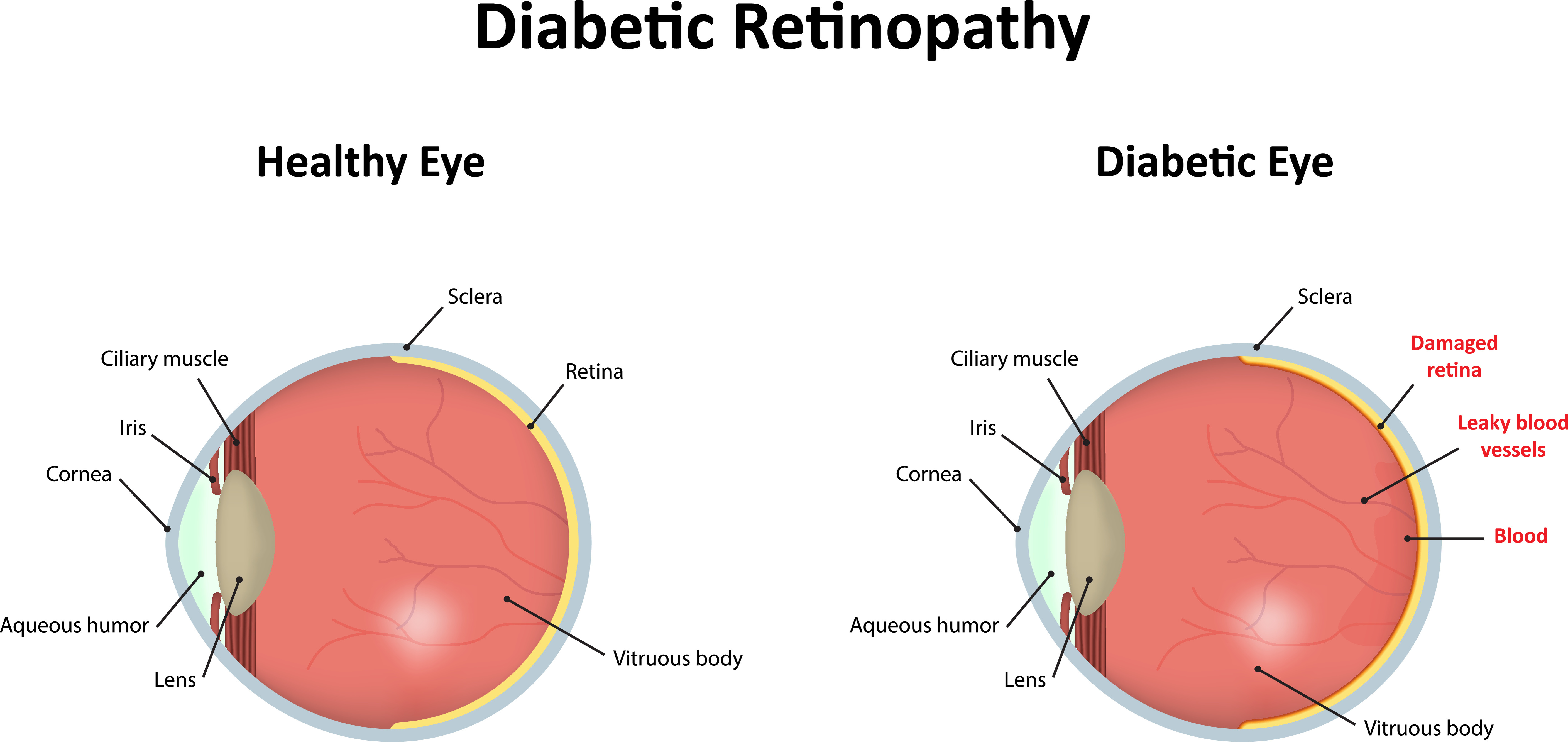
Eye health is one of the biggest concerns for people with diabetes. Over time, a continuously high blood sugar level damages the tiny blood vessels in the retina. This leads to a disease called diabetic retinopathy.
The retina is the light-sensitive layer of neural cells lining the back of the eye. It converts light rays into electrical signals, which get sent to the brain via the optic nerve. The brain processes these signals into images that you can see.
The retina can't work properly without a constant supply of fresh blood. That’s why the damaged blood vessels caused by elevated blood sugar seriously threaten your vision.
What Is Diabetic Eye Disease?
Diabetic eye disease describes a group of eye conditions that can develop in people with diabetes. The most common health issues affecting the vision of diabetics include:
Diabetic Retinopathy
Diabetic retinopathy is the leading cause of vision loss in American adults aged 20 to 74.5 It’s also one of the most common and severe diabetes complications.3
It causes damage to the small blood vessels in the retina. There are usually no symptoms in the early stages of diabetic retinopathy, but without treatment, it can eventually lead to blindness.
Diabetic Macular Edema
Diabetic macular edema (DME) occurs when the macula of the eye swells due to fluid accumulation. The macula is the area of the retina that contains a high concentration of cells that provide sharp central vision.
You might notice issues with reading or driving if you are developing DME. Other symptoms include blurry vision and distortion in the vision.
Cataracts
A cataract occurs when the usually clear lens of the eye becomes cloudy. People with diabetes are more likely to develop cataracts. They’re also more likely to get cataracts at a younger age.
Cataracts cause cloudy or hazy vision and dull colors.
Glaucoma
Glaucoma is a group of diseases that cause high pressure inside the eye. The increased pressure squeezes the blood vessels that serve the retina and optic nerve. This leads to vision loss.
Diabetic retinopathy can cause neovascular glaucoma. This type of glaucoma causes abnormal new blood vessels to grow between the iris and the cornea of the eye.
Glaucoma symptoms include:
- Blurred vision
- Double vision
- Headaches
- Eye pain
Retinal Detachment
Retinal detachment is an eye health emergency in which the retina pulls away from its normal position. This causes the retinal cells to separate from the blood vessels that provide oxygen and nourishment. Left untreated, even for a short time, it can cause blindness.
Symptoms of a detached retina include:
- Floaters
- Flashing
- Reduced vision
- Shadows or curtains over your vision
What Are the Symptoms of Diabetic Eye Disease?
Usually, there are no symptoms in the early stages of diabetic retinopathy. Many people with early diabetic retinopathy don’t know they have it until they get an eye exam.
As the condition progresses, you may experience:
- Floaters (spots or strings you see floating in your field of vision that aren’t there)
- Blurry vision
- Impaired color vision
- Dark or empty spots in your field of vision
- Vision loss
How Is Diabetic Eye Disease Diagnosed?
An eye doctor can diagnose diabetic eye disease with a comprehensive eye exam. They may perform a dilated eye exam to examine your retina. They will look for:
- Growth of abnormal blood vessels
- Fatty deposits or any swelling in the retina
- Scar tissue
- Bleeding in the retina or into the vitreous
- Abnormalities in your optic nerve
- Retinal detachment
Your eye doctor will also check your vision and measure the pressure in your eye. Depending on your needs, they may recommend additional tests.
Types of Diabetic Retinopathy
There are two types of diabetic retinopathy:
Early or Non-Proliferative Diabetic Retinopathy
This is the most common form of diabetic eye disease. Instead of new blood vessels forming, the existing blood vessels in the retina grow weak and leak fluid and blood into the retina. Swelling and dilation of the blood vessels might also occur.
This form of diabetic retinopathy can range from mild to severe.
Advanced or Proliferative Diabetic Retinopathy
Over time, diabetic retinopathy leads to the proliferation of new blood vessels. These poorly formed blood vessels are prone to leakage, and eventually, scar tissue will begin to grow. Advanced diabetic retinopathy increases a person’s risk for retinal detachment.
Who Is At Risk of Developing Diabetic Eye Disease?
Anyone with diabetes is at risk of developing diabetic eye disease. However, some factors increase the risk of vision problems, including:
- Duration of the disease (over time, the risk of eye health problems increases for people with diabetes)
- Persistently high blood sugar levels
- High blood pressure and cholesterol levels
- Tobacco use
- Pregnancy
Treatment for Diabetic Eye Disease
After your doctor determines the type and severity of your diabetic eye disease, they will recommend the appropriate treatment.
For early diabetic retinopathy, treatment may only involve monitoring your eye health with more frequent exams and managing your blood sugar levels.
Treatment for advanced diabetic retinopathy and other types of diabetic eye disease may include:
Medication
Vascular endothelial growth factor (VEGF) inhibitors can be injected directly into the eye to prevent the growth of abnormal blood vessels. Growth inhibitor medication can be used alone or in combination with other treatments.
Focal Laser Treatment
Also called photocoagulation, this is a laser treatment that seals leaky blood vessels. It slows or stops liquid from seeping into the eye.
Laser treatment might not return your vision to normal, but it can reduce the risk of worsening macular edema.
Anti-VEGF therapy has replaced focal laser as the primary treatment for diabetic macular edema.
Scatter Laser Treatment
Also called panretinal photocoagulation (PRP), this procedure shrinks abnormal blood vessels. It might result in a loss of some peripheral or night vision, but it slows or stops the damage caused by abnormal blood vessels.
Vitrectomy Surgery
The vitrectomy removes blood and scar tissue from the middle of the eye through a small incision. Vitrectomy surgery might be an option to slow or stop the progression of diabetic retinopathy.

Cataract Surgery
This common surgical procedure involves removing and replacing the clouded lens with an artificial lens implant.
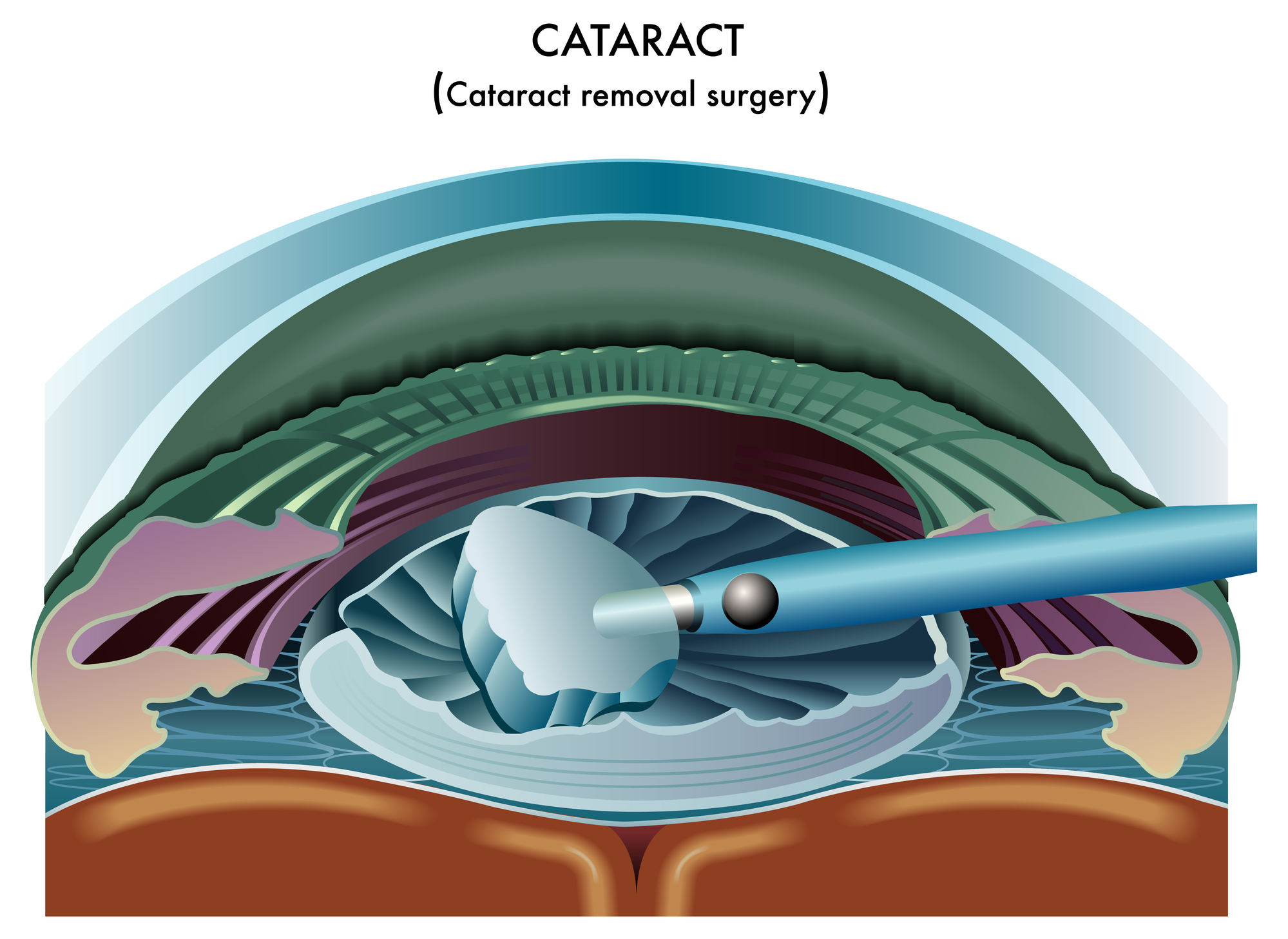
Most people who get cataract surgery have better vision afterward. However, improved eyesight depends on treating any damage from macular edema or diabetic retinopathy.
How to Prevent Diabetic Eye Disease
There are things you can do to reduce your risk for diabetic eye disease and prevent it from getting worse. These include:
- Getting routine eye exams
- Controlling your blood sugar levels
- Managing your blood pressure and cholesterol
- Scheduling an eye exam as soon as you notice any vision changes
- Quitting smoking if you smoke
- Taking a glycosylated hemoglobin (hemoglobin A1C) test, which estimates your risk for complications based on your recent blood sugar levels
Summary
Diabetes is a chronic condition that causes high blood glucose levels. High blood glucose levels damage the blood vessels in the eye and cause diabetic eye disease.
Diabetic retinopathy is the most common and severe form of diabetic eye disease. It often causes no symptoms in its early stages, so routine eye exams are critical.
You can help prevent diabetic eye disease by managing your blood sugar, blood pressure, and cholesterol levels.
In this article
6 sources cited
Updated on February 20, 2024
Updated on February 20, 2024
About Our Contributors
Kelly Brown, a content writer for Vision Center, is dedicated to sharing vital information to assist individuals in making informed decisions about their vision health. Her writing covers a range of topics, from selecting the best eye doctor to addressing health issues impacting vision, with the aim of educating readers through informative and engaging content.
Dr. Melody Huang is an optometrist and freelance health writer with a passion for educating people about eye health. With her unique blend of clinical expertise and writing skills, Dr. Huang seeks to guide individuals towards healthier and happier lives. Her interests extend to Eastern medicine and integrative healthcare approaches. Outside of work, she enjoys exploring new skincare products, experimenting with food recipes, and spending time with her adopted cats.

