Updated on September 24, 2024
What to Know about Corneal Transplant Surgery


Vision Center is funded by our readers. We may earn commissions if you purchase something via one of our links.
What is Corneal Transplant Surgery?
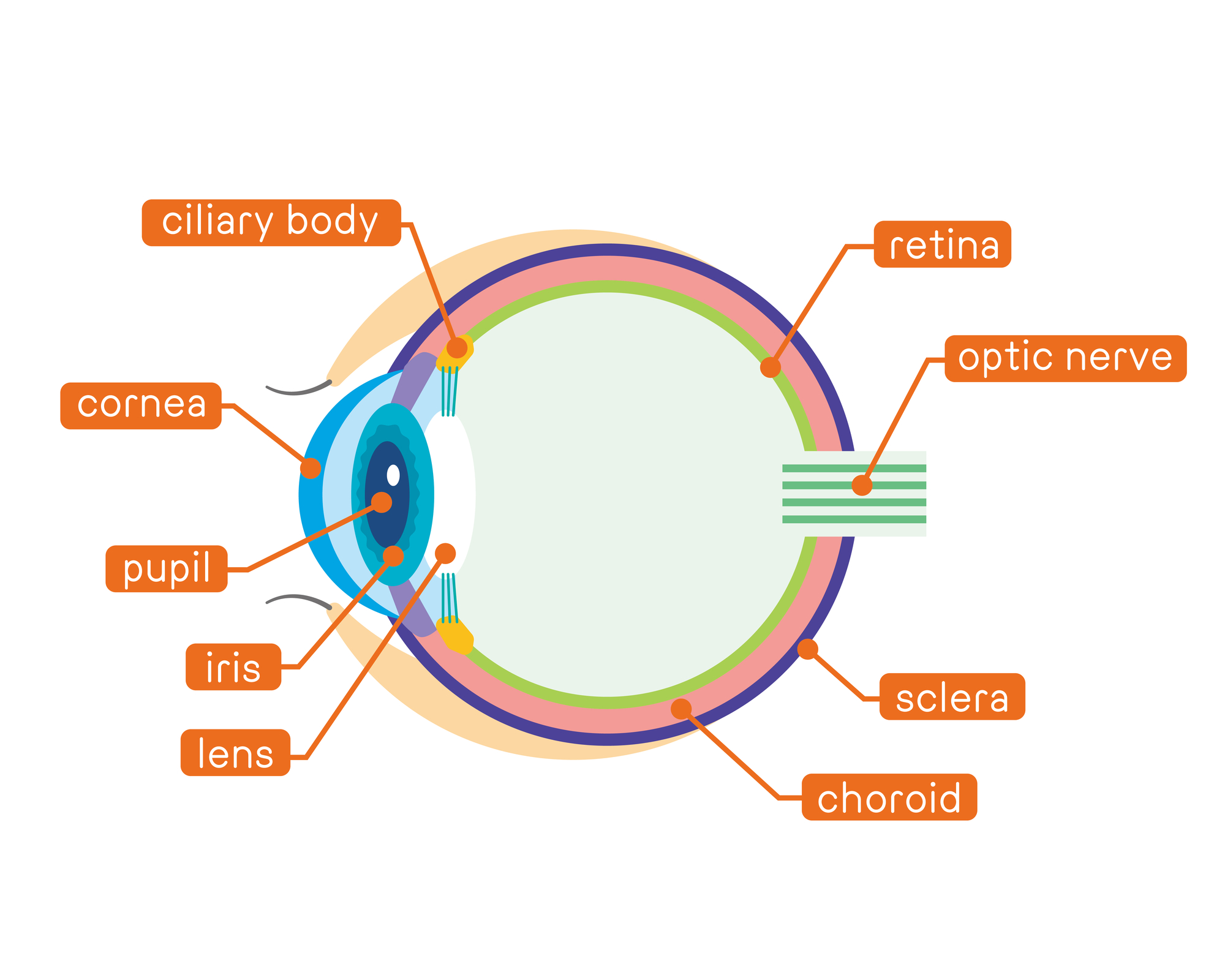
Corneal transplant surgery is medically referred to as a form of keratoplasty. It involves removing diseased or damaged corneal tissue and replacing it with donor corneal tissue.
The cornea is vital to your ability to see. It allows light to enter into the eye.
There were over 49,000 corneal transplant procedures in the United States in 2021. Many were successful, with only a third of the risk of rejection in full-thickness transplants.1
Who Needs Cornea Transplant Surgery?
You may require corneal transplant surgery if you have a damaged cornea that’s causing blurred vision, cloudy vision, or eye pain.

Conditions indicating a damaged cornea include:
- Fuch’s Dystrophy. Dead or dysfunctional endothelial cells result in a swollen cornea and blurred vision
- Keratoconus. Thin and bulging cornea
- Bullous keratopathy. Blister-like swelling of the cornea
- Keratitis. Corneal inflammation caused by bacteria, fungi, or parasites
- Infection or injury. Can lead to cornea scarring
What to Expect Before Surgery
Before undergoing corneal transplant surgery, there are several important steps and precautions that you must know and take:
1. Consultation with the Ophthalmologist
The ophthalmologist will assess your condition by conducting a physical examination and reviewing your medical history. During this time, you can discuss your damaged or diseased cornea and ask questions.
2. Pre-Surgical Evaluations and Requirements
Your surgeon will order routine lab work to rule out underlying medical conditions that might complicate the surgery. It’s crucial to inform your doctor about all your medications.
These include prescription and over-the-counter (OTC) drugs. You can expect to discontinue certain medications, such as blood thinners, before the surgery to minimize surgical risks.
3. Surgery Planning
After deciding to proceed with the surgery, you and your doctor will set a date for the operation. The surgery date might change if compatible healthy donor tissue isn’t available.
4. Pre-Operative Preparations
Your doctor will prescribe antibiotic eye drops you’ll use the day before the surgery to reduce the risk of postoperative infections.
Since corneal transplant surgery is an outpatient procedure, you need to plan for transportation, as you’ll not be able to drive immediately after the surgery.
5. The Day of Surgery
From arrival to the completion of the procedure, here's what you’ll typically experience:
- Arrive at the facility and complete all necessary paperwork
- Receive numbing drops in your eye and medication for relaxation before surgery
- Undergo sedation or general anesthesia to prevent movement and pain
- Have a device placed to keep your eye open during the procedure
- Possibly receive treatment for additional eye problems, like cataracts, during the cornea transplant6
What to Expect After Surgery
After a corneal transplant, there are several postoperative steps and precautions you'll need to follow to ensure a smooth recovery.
Here's a summary of what you can expect:
- Wear an eye patch for 1 to 4 days to protect the eye and reduce infection risk
- Move to a recovery room post-surgery for close monitoring
- Go home after recovery, assisted by someone else for the drive
- Use prescribed eye drops to reduce inflammation and prevent infection
- Take pain medication as necessary for eye discomfort
- Expect some redness, light sensitivity, and discomfort in the eye as it heals
- Be able to drive 24 hours post-transplant, with specific guidance from the doctor on returning to work
- If the job is physically demanding, take a longer time off work
- Avoid activities that could lead to a direct hit to the eye
Contact Lenses After Surgery
Following keratoplasty, you may need contact lenses for vision or preference reasons.7 Contact lenses can correct:
- Irregular astigmatism
- High regular astigmatism
- High anisometropia
- Secondary aniseikonia
- Simple ametropia
Rigid gas-permeable contact lenses might be helpful following penetrating keratoplasty. You might also need them after deep anterior lamellar keratoplasty surgery.8
Recovery Timeline After Cornea Transplant Surgery
A full recovery following cornea transplant surgery can take upwards of one year, if not longer. You can expect blurred vision in the days, weeks, and months following surgery.
Full vision can take up to one year to return as cornea transplants are invasive procedures. You may experience swelling, inflammation, and sensitivity to light as your eye recovers and heals.5
Many people who receive corneal transplants experience good vision for years to come, especially when they closely follow all post-op instructions.
What are the Types of Corneal Transplants?
There are three main types of corneal transplants:
1. Endothelial Keratoplasty
You may benefit from an endothelial keratoplasty procedure if you have a damaged endothelium, the cornea’s innermost layer. The two common types of endothelial keratoplasty are:
- Descemet’s stripping automated endothelial keratoplasty
- Descemet’s membrane endothelial keratoplasty (DMEK)
How it Works
An eye doctor (ophthalmologist) removes the damaged innermost tissue during this cornea transplant procedure. They also provide a graft to replace it with healthy donor tissue.
Rather than using several stitches, your doctor uses a small air bubble to maintain the placement of the donor tissue.
Side Effects
Although this donor cornea procedure bears a relatively low risk, possible side effects include:
- Bleeding
- Infection
- Glaucoma
- Retinal detachment
- Tissue rejection
Cost
Endothelial keratoplasty, more specifically Descemet's stripping endothelial keratoplasty (DSAEK), costs a little more than $9,300.2 Though this type of cornea transplantation is quite costly, it’s less expensive than other donor cornea transplant surgeries.
2. Penetrating Keratoplasty
Penetrating keratoplasty is ideal if you have a significant corneal injury and need to replace all layers of your cornea. This procedure is a full-thickness corneal transplant.
How it Works
During this operation, a surgeon carefully removes the cornea with a scalpel. Afterward, they replace and attach all layers with fragile, hair-like stitches.
Side Effects
This surgery has a longer recovery time and more risks than others. These risks include:
- Endophthalmitis (infection within the eye)
- Endothelial failure (a type of coronary artery disease)
- Glaucoma (damage to the optic nerve)
- Microbial keratitis (inflammation of the cornea caused by bacteria or fungi)
- Wound leaking (fluid leaking from the incision site)
- Transplanted tissue rejection (your body's immune system attacks the new cornea)
Cost
Penetrating keratoplasty costs approximately $10,239. However, this procedure requires the replacement of far more tissue than those mentioned above.3
3. Deep Anterior Lamellar Keratoplasty (DALK)
If you have keratoconus or a bulging cornea, you may benefit from deep anterior lamellar keratoplasty (DALK). This is the partial thickness corneal transplant.
This surgery treats damage to the front and middle layers of the cornea. It also restores healthy corneal tissue.
How it Works
In anterior lamellar keratoplasty, a surgeon dissects the cornea into two small pieces to easily remove the damaged front and central areas. Through tedious stitching, they remove and attach healthy donor corneal tissue.
Side Effects
Compared to penetrating keratoplasty, DALK cornea transplants offer significant safety advantages. This is because doctors open and expose far less of the eye during surgery.
A few complications include:
- Incomplete attachment of Descemet’s membrane
- Opacification of the interface between the posterior corneal stroma and Descemet’s membrane
- Infection
Cost
Anterior lamellar keratoplasty corneal transplantation costs nearly $9,920.4
What are the Risks of Corneal Transplants?
Many corneal transplant surgeries in the United States are successful. However, there are still a few risks of these types of procedures, including:
- Bleeding
- Infection
- Glaucoma
- Retinal detachment
- Cornea detachment
- Fluid leakage from the cornea
- Vision acuity issues, such as vision sharpness
How Common is Graft Rejection After Corneal Transplant?
Between 18% to 21% of graft recipients experience cornea rejection after their transplant. When rejection happens, the success rate of reversing the episode ranges from 50% to 90%.9
Rejection following deep anterior lamellar keratoplasty is rare. Steroids can treat cornea transplant rejection if they begin early upon symptom onset.
What is the Prognosis of Corneal Transplants?
The prognosis for cornea transplants depends on many factors, including:
- The exact cause of cornea damage
- The type of surgical technique your surgeon uses
- Your immune system’s acceptance of the donated cornea
Discuss your post-op outlook one-on-one with your ophthalmologist before surgery. Contact your ophthalmologist if you have any concerns regarding your vision following your cornea transplant surgery.
Summary
Corneal transplant surgery can be a life-changing procedure for those suffering from severe corneal damage or disease. While there are some risks, most experience better vision and quality of life after their procedure.
Follow all pre- and post-operative instructions closely to ensure a successful outcome. Consult your ophthalmologist to learn more about corneal transplant surgery and if it’s right for you.
In this article
9 sources cited
Updated on September 24, 2024
Updated on September 24, 2024
About Our Contributors
based information about eye care. Our team, comprising doctors, researchers, and writers, is dedicated to our mission of delivering accurate and reliable visual health content, constantly creating, publishing, and updating to ensure the highest quality of information.
Dr. Melody Huang is an optometrist and freelance health writer with a passion for educating people about eye health. With her unique blend of clinical expertise and writing skills, Dr. Huang seeks to guide individuals towards healthier and happier lives. Her interests extend to Eastern medicine and integrative healthcare approaches. Outside of work, she enjoys exploring new skincare products, experimenting with food recipes, and spending time with her adopted cats.

