Updated on October 22, 2024
What to Expect After Keratoconus Surgery


Vision Center is funded by our readers. We may earn commissions if you purchase something via one of our links.
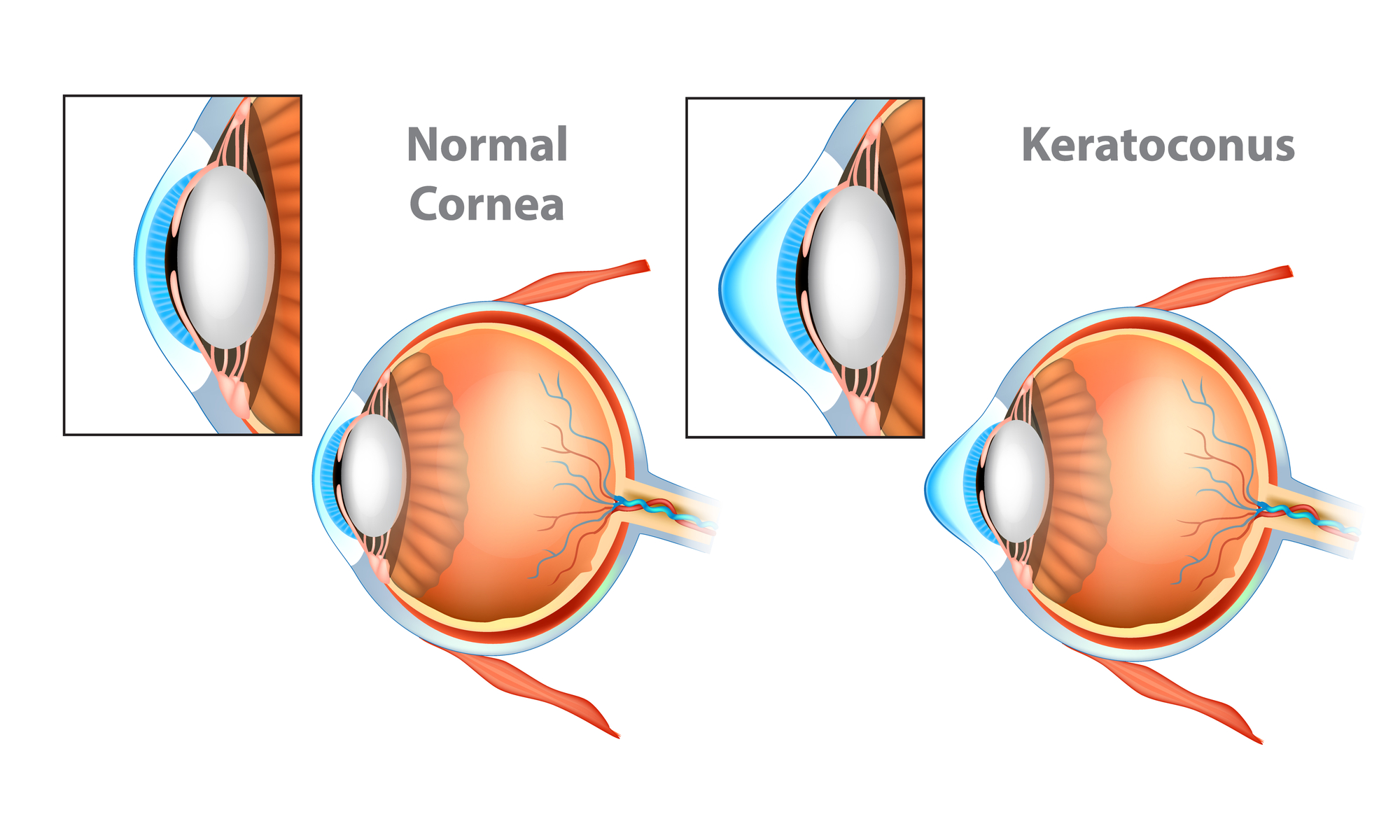
Keratoconus is a degenerative condition that affects the cornea (the clear front layer of the eye). It gradually thins and distorts the cornea, leading to vision and refractive errors.
The condition commonly affects both eyes, although one eye may be affected more than the other. It typically affects people ages 10 to 25 and progresses over several years.
The condition can worsen if left untreated, leading to severe vision problems or vision loss. However, early diagnosis and keratoconus treatments can help slow progression, preventing further vision loss.
In this article, we cover the symptoms of keratoconus and the treatment options available.
What Causes Keratoconus?
The exact cause of the condition isn't well understood. However, some eye experts believe it's linked to genetics.1
Although keratoconus is more common among people between ages 10 and 25, you can be at risk of developing it regardless of age. There are also other possible causes, such as:
- Vigorous eye rubbing
- Atopy (genetic predisposition to develop allergies)
Different Stages of Keratoconus
Keratoconus has four stages, which are:
- Early keratoconus. The earliest stage of keratoconus has little to no symptoms or effects on your vision
- Moderate keratoconus. The changes to your corneal shape become more apparent during this stage
- Advanced keratoconus. You will likely have substantial corneal thinning and scarring at this stage
- Severe keratoconus. Causes severe or dramatic corneal distortion, scarring, and thinning
What Are the Symptoms of Keratoconus?
Corneal changes due to keratoconus can make it difficult for the eye to focus even while using glasses or soft contact lenses. Some common signs of keratoconus include:
- Irregular astigmatism
- Distorted or blurred vision
- Glares and halos in bright light
- Sensitivity to light
- Eye irritation
- Headaches due to eye pain
Preparing for Keratoconus Surgery
How you prepare for keratoconus surgery depends on the specific procedure you will undergo. However, there are general rules for most eye surgeries.
If you’re preparing for surgical keratoconus treatment, you must:
- Stop using your prescription eyeglasses or contact lenses a few days or weeks before surgery
- On the day of the surgery, do not use eye makeup, such as mascara, eyeliners, or fake eyelashes, as they can breed bacteria
- Don’t wear perfume or after-shave
- Eat a light meal and drink fluids beforehand
- Prepare reliable transportation to and from surgery, as you’ll have impaired vision immediately after
- Follow your doctor’s instructions carefully and discuss any concerns beforehand to ensure you’re ready for the procedure
After the procedure, you should schedule a follow-up visit within 24 to 48 hours. Keep your surgeon informed on any changes or reactions to the surgery during the healing process.
Should You Get Surgery for Keratoconus?
Not everyone needs invasive surgery to manage their keratoconus. During the early stages of keratoconus, you can enhance your vision with contact lenses or prescription glasses.
Noninvasive options, such as scleral lenses, can also significantly reduce the need for surgery.3 Scleral lenses are contact lenses placed on the sclera (white of the eye) and enclose the cornea without touching it. This boosts vision and improves comfort by covering the bulging cornea.
However, severe keratoconus requires more intense interventions. Besides surgical options, such as a corneal transplant (keratoplasty), you may also get gas-permeable contact lenses.2
Listen In Q&A Format
What To Expect After Keratoconus Surgery
Vision Center Podcast
Keratoconus Treatment Options
Once the condition worsens, you may need surgery to treat its symptoms. Different surgical options are available as keratoconus treatment options, which include:
1. Corneal Cross-Linking (CXL)
Corneal cross-linking is a new technique that uses a special eye drop and ultraviolet (UV) light to strengthen the cornea’s collagen fibers. It aims to prevent further progression of keratoconus by using collagen fibers to stabilize corneal tissue. Stronger collagen fibers also reduce or eliminate the need for a transplant.
Corneal crosslinking is very effective, with a 95% success rate. Few keratoconus patients experience adverse vision changes after corneal crosslinking. If this occurs, you can seek a repeat procedure.
Candidacy
You’re a good candidate for corneal crosslinking if you:
- Have early-stage keratoconus
- Have a cornea that’s not too thin
- Are between 15 and 25 years of age
- Are generally healthy and have no underlying health conditions
- Do not have any other eye diseases, such as cataracts
- Do not have any corneal scarring due to trauma or previous surgery
Procedure
Corneal cross-linking is a minimally invasive procedure done in two ways:
- Epithelium-off crosslinking. This involves corneal epithelium removal and uses riboflavin (vitamin B2) to help strengthen collagen fibers. Riboflavin provides a healthy environment for forming new, stiff, and strong collagen fibers.
- Epithelium-on method. Also known as transepithelial crosslinking, this procedure does not involve corneal epithelium removal. This prevents the risk of infection and discomfort. Currently, only epithelium-off crosslinking performed with a Glaukos KXL System is FDA-approved.

The recommended topical treatments used during CXL surgery include Photrexa® Viscous and Photrexa®.4 The entire procedure should take around 1 to 2 hours.
Post-Op Care
Your surgeon will give you post-op care instructions to promote healing. Your doctor may also include antibiotics and pain medication to prevent infection or discomfort after surgery.
Side Effects and Risks
Some potential side effects and complications include:
- Eye infections
- Eye pain
- Swelling
- Corneal or epithelial damage
- Blurring vision (temporary)
- Delayed healing
- Corneal scarring
Cost
On average, corneal crosslinking costs about $2,500 to $4,000 per eye. If it’s beyond what you can afford now, insurance coverage is available because the procedure is considered medically necessary.
However, you should talk to your surgeon and insurance provider about the procedure’s cost. This is because the total amount may differ from one surgeon to another.
2. Topography-Guided Conductive Keratoplasty (CK)
Topography-guided conductive keratoplasty (CK) is a noninvasive procedure that uses radiofrequency energy to reshape irregular corneas. It’s also valuable for treating low hyperopia with or without astigmatism and presbyopia (age-related farsightedness).
According to the American Academy of Ophthalmology, Topography-guided CK can also treat residual refractive errors after cataract surgery or LASIK.5 Overall, the procedure takes 5 minutes or less to complete.
However, the procedure is not suitable for people who:
- Are breastfeeding
- Have a history of keratitis
- Are immunocompromised
- Have eye diseases, such as dry eyes
- Have corneal scarring within the central optical zone
- Use a pacemaker, which can be affected by radio waves
Candidacy
You’re a good candidate for topography-guided CK if you:
- Are 40 years or older
- Measure between +0.75 and +2.50 diopters of correction
- Have lower than 0.75 diopters of astigmatism
- Have presbyopia (age-related farsightedness)
Procedure
Your surgeon performs the CK procedure through computer-guided topographic images of your cornea using special imaging technology. This helps individualize your treatment based on specific needs.
Your surgeon will mark your visual axis with a device known as a Sinskey Hook to mark the cornea in the areas to be treated. Then, the keratoplast tip is inserted into the marked areas, which sends a mild radiofrequency energy into your cornea. This gently heats the cornea's upper layer, shrinks it to improve the corneal shape, and enhances refractive power.
Post-Op Care
After the treatment, your surgeon will administer antibiotic drops in the area and place a soft contact lens on your eye to protect it as it recovers. They will also give you post-operative care instructions to ensure proper healing.
Most people achieve a 20/40 vision or better immediately. Others take a few weeks to notice positive changes.
Side Effects and Risks
Common side effects include:
- Photophobia (sensitivity to light)
- A gritty feeling in your eyes that wears off with time
- Visual fluctuation
- Slight nearsightedness
- Corneal regression requiring a repeat procedure
Rare complications include:
- Corneal aseptic stromal necrosis
- Surgically induced astigmatism
Cost
On average, CK procedures cost about $1,500 to $2,000 per eye. Because it's considered an elective surgery, it's not covered by insurance.
The cost of topography-guided CK will vary depending on your:
- Location
- Facility
- Surgeon’s experience
3. Penetrating Keratoplasty (Corneal Transplant Surgery)
Penetrating keratoplasty (PK) is a century-old procedure and the most commonly performed eye transplant. It treats corneal problems that affect visual acuity, such as keratoconus.
The procedure involves completely removing a damaged section of the cornea and replacing it with a healthy one from a donor. In some cases, the cornea may be artificially bundled with the donor tissue (keratoprosthesis).6
The risk of permanent vision loss from the latter stages of keratoconus makes it a serious cause for concern. Although PK is a common eye surgery, it’s only recommended in severe and advanced keratoconus.
Candidacy
You’re a good candidate for PK if you have:
- A thin, cone-shaped cornea (keratoconus)
- A corneal injury
- Unhealthy corneal tissue due to ulcers or sores
Procedure
Before the procedure, your surgeon will conduct a comprehensive examination of your cornea to determine if PK will work for you. To avoid infections, you’ll also have to use antibiotic eye drops a day before PK.
The entire procedure typically takes about 30 minutes to an hour. During surgery, your surgeon will administer anesthesia to ease discomfort and a sedative to keep you calm.
Using a device known as a trephine, your surgeon will then make a full-thickness incision in your cornea and safely remove the damaged section. Then, they’ll replace your cornea with a healthy one from a donor.
Post-Op Care
Your doctor will likely give you an eye shield to protect your healing cornea for a few days. Post-op care instructions to promote recovery will also be provided.
Side Effects and Risks
Some risks and side effects of PK include:
- Corneal stromal graft rejection
- Infection
- Glaucoma (increased eye pressure)
- Clouding of the eye lens
- Swollen cornea
- Retinal detachment
- Corneal scarring
Cost
On average, PK costs about $1,500 to $2,500 per eye. If PK is considered medically necessary, private coverage or Medicare will cover some costs. You may still have to pay out of pocket for specialty and hospital copays.
4. Deep Anterior Lamellar Keratoplasty (DALK)
Deep anterior lamellar keratoplasty (DALK) is a procedure for advanced keratoconus. It reduces the risk of transplant rejection and is more complex than PK.
Unlike PK, DALK partially removes the affected corneal stroma and replaces it with a healthy donor. This surgical procedure preserves Descemet’s membrane and endothelium.8 These are the two layers of the cornea that lie underneath the corneal stroma.
If Descemet’s membrane and endothelium are left intact, the wound is less delicate and less prone to transplant rejection. A study found that DALK patients have a graft survival rate of over 90%.9
Candidacy
You’re an ideal candidate for DALK if you have:
- Keratoconus
- A corneal injury
- Unhealthy corneal tissue due to ulcers or sores
Procedure
The DALK procedure is similar to penetrating keratoplasty, except it preserves the endothelium and Descemet’s membrane. The donor cornea has the endothelium-Descemet’s membrane removed. Then, the graft is placed within the recipient’s membrane.
The graft is secured with stitches, which can be removed post-surgery. The procedure usually takes about an hour or less.
Post-Op Care
Topical corticosteroids and antibiotics are administered after the operation. Your doctor will also monitor you for any problems, including:
- Inflammation
- Infection
- Graft rejection
- Astigmatism
- Suture-related problems
Side Effects and Risks
Some risks and side effects of DALK include:10
- Perforation of Descemet’s membrane during surgery
- Graft rejection (rare compared to PK)
- Corneal swelling
- Infection in the healing area
- Posterior scarring
Cost
The DALK procedure costs roughly $13,000 for an outpatient procedure and about $28,000 for an inpatient procedure. The cost may vary based on your location, facility, and the surgeon’s experience. Also, insurance will likely cover most of the cost.
Alternative Treatment Options
Apart from scleral contact lenses, there are other alternatives to keratoconus surgery. These include:
- Eyeglasses or soft contact lenses. These correct vision issues in early keratoconus
- Gas permeable contact lenses (GP lenses). The smooth, uniform refracting surface of GP lenses replaces the uneven curvature of the cornea, improving comfort and visual acuity
- Intacs. Intacs are plastic, arc-shaped corneal implants placed in the cornea to restore its shape
- Piggyback lenses. These are hard contact lenses placed on soft ones to improve comfort
- Hybrid contact lenses. These have a rigid center with a soft ring on the edges to increase comfort
- Prosthetic lenses. These lenses fix corneal irregularities. They’re specially designed through 3D imaging to match the exact impression of your sclera.
Summary
Keratoconus is a degenerative condition that affects the cornea (the clear front layer of the eye). It gradually thins and distorts the cornea, leading to vision and refractive errors.
Although the condition isn't well understood, experts believe keratoconus is linked to genetics. The condition has four stages, with symptoms that worsen as it progresses.
Not everyone needs surgical treatment for keratoconus. However, more invasive surgical options may be necessary for treating keratoconus in its advanced or severe stages. Consult your doctor for a proper diagnosis and to confirm which treatment will be best for you.
In this article
10 sources cited
Updated on October 22, 2024
Updated on October 22, 2024
About Our Contributors
Vincent Ayaga is a medical researcher and seasoned content writer with a bachelor's degree in Medical Microbiology. Specializing in disease investigation, prevention, and control, Vincent is dedicated to raising awareness about visual problems and the latest evidence-based solutions in ophthalmology. He strongly believes in the transformative power of ophthalmic education through research to inform and educate those seeking knowledge in eye health.
Dr. Melody Huang is an optometrist and freelance health writer with a passion for educating people about eye health. With her unique blend of clinical expertise and writing skills, Dr. Huang seeks to guide individuals towards healthier and happier lives. Her interests extend to Eastern medicine and integrative healthcare approaches. Outside of work, she enjoys exploring new skincare products, experimenting with food recipes, and spending time with her adopted cats.

