Updated on June 20, 2025
What Are Intacs? (Corneal Implants)


Vision Center is funded by our readers. We may earn commissions if you purchase something via one of our links.
If you've recently learned you have keratoconus, you might wonder if those Intacs can permanently fix your vision.
This article clears up how Intacs work, their benefits, limitations, risks, and what costs to expect.
How Do Intacs Work?
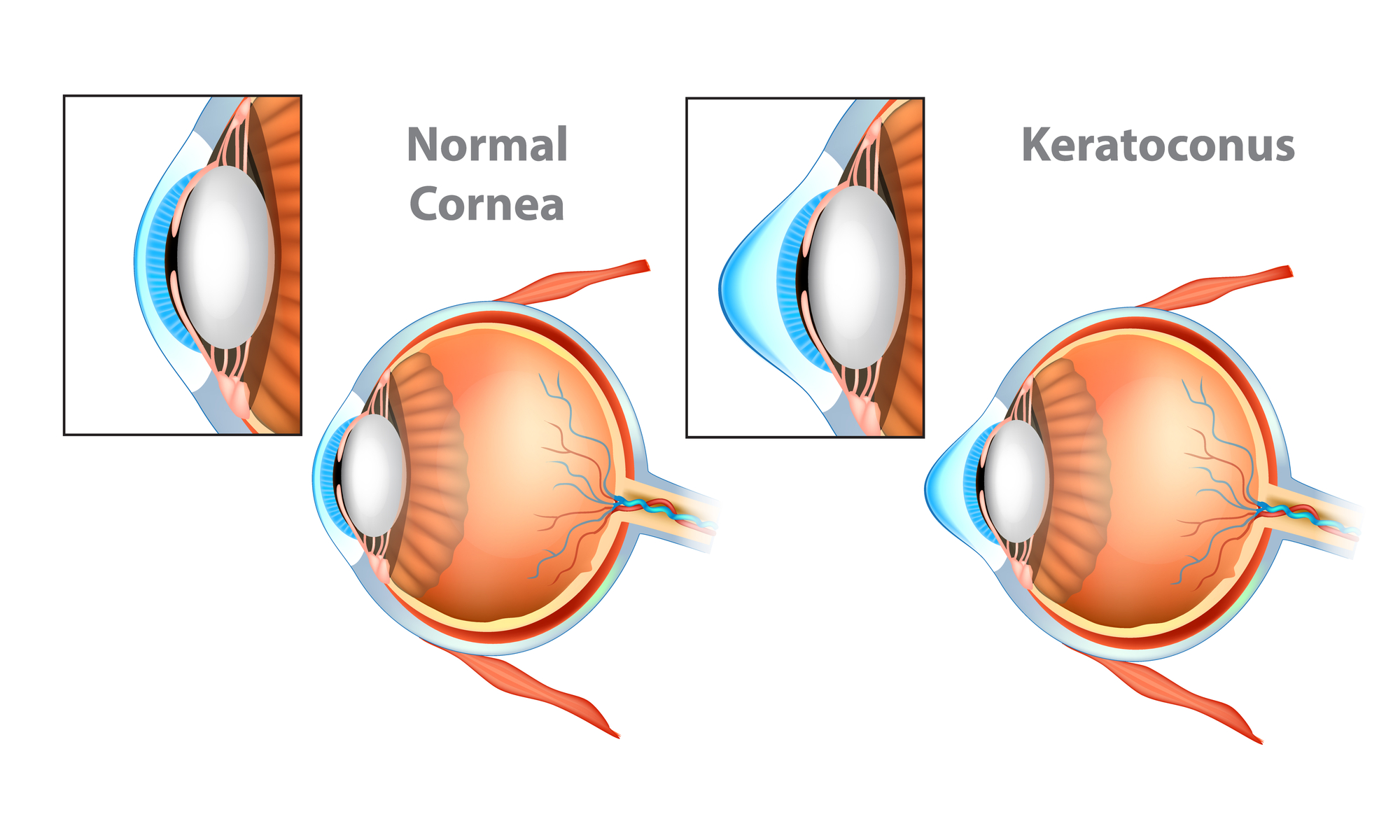
Intacs are small, semicircular implants made of biocompatible plastic (PMMA) placed within your cornea (intrastromal corneal segments).
They reshape the cornea by gently flattening its cone-like shape from the periphery, regularizing the corneal stroma to improve your vision.
Unlike a corneal transplant, Intacs don't replace corneal tissue; they're additive, reversible supports.
Here's a quick comparison of common keratoconus treatments:
| Treatment | How it Works | Goal | Tissue Impact |
| Intacs | Reshapes the cornea mechanically | Improve shape and vision | Additive |
| Cross-linking | Strengthens collagen structure | Halt disease progression | Stabilizing |
| Transplant | Replaces damaged cornea | Restore clear vision | Replacement |
Who is a Good Candidate for Intacs?
To ensure Intacs will help you, your doctor checks several factors. Ideal candidates typically have:
- Moderate keratoconus (maximum curvature less than 55 diopters)
- Corneal thickness of at least 450 microns
- Clear central cornea (no major scars)
- Contact lens intolerance (difficulty wearing contacts comfortably)
- Realistic goals (Intacs improve, but don't fully correct vision)
Intacs Alternatives and Combo Treatments Worth Discussing
Intacs aren’t your only option. Here’s a quick comparison of common treatments:
| Treatment | Purpose | Best for |
| Collagen cross-linking (CXL) | Stabilize and halt keratoconus progression | Young, actively progressing keratoconus |
| Scleral lenses | Mask corneal irregularity | Non-surgical improvement of functional vision |
| Corneal transplant (DALK) | Replace severely damaged corneal tissue | Severe keratoconus unresponsive to other treatments |
Many keratoconus specialists recommend combining Intacs with corneal collagen crosslinking. Intacs improve your vision while cross-linking prevents further progression, offering long-term stability.
However, you should always ask your surgeon if combining treatments suits your situation.
What Does Intacs Surgery Look Like?
Getting Intacs is an outpatient surgical procedure, typically taking just 15 minutes. Here's how your surgery day unfolds:
- Topical anesthesia. Your eyes get numbing drops—no general anesthesia required.
- Preparation. Your cornea is gently marked to guide precise implant placement.
- Channel creation. A femtosecond laser (preferred for safety and accuracy) creates tiny tunnels for the Intacs.
- Intacs insertion. The ring segments slide neatly into the laser-created tunnels.
- Closing the incision. Usually self-sealing; occasionally, a small stitch is added.
- Home recovery. You go home the same day with clear instructions and medicated drops.
What is Recovery After Intacs Surgery Like?
Recovery after Intacs surgery follows clear milestones, and while your vision might fluctuate initially, patience and good aftercare pay off.
- In the first few days, your eyes may feel scratchy and sensitive to light. Vision is typically blurry at first but gradually clears.
- After one week, discomfort usually eases significantly. You can often resume normal daily activities, though you must avoid strenuous exercise, rubbing your eyes, or getting water in them.
- By about three months, your vision stabilizes enough for new glasses or contact lenses. Expect noticeable improvements, though minor fluctuations are normal during healing.
For many patients, Intacs significantly enhance night vision by reducing distortions. Daily activities, including driving, reading, and screen time, typically become easier and more comfortable.
When you get fitted for new contacts, mention your Intacs implants to ensure the best fit and comfort.
What are the Benefits of Intacs?
Studies consistently show meaningful vision improvements after Intacs, though gains depend on disease severity:
- Average improvement. Many gain 1 to 2 lines on a vision chart in best-corrected visual acuity (BCVA).
- Easier correction. Reduced corneal irregularity typically makes glasses or contacts more comfortable.
- Contact lens tolerance. Patients previously intolerant to contact lenses often find lens wear significantly easier after Intacs.
Even with these improvements, most patients still need some form of vision correction post-surgery.
What are the Risks of Intacs?
While Intacs are generally safe, being aware of potential complications helps set realistic expectations.
Low-but-real complications include:
- Infection. Rare, treatable with prompt medical attention (<1%).
- Glare and halos. Usually mild; more noticeable at night.
- Ring extrusion. Segments pushing through the corneal surface; more likely if placed too superficially (2 to 6%).
- Revision or removal. Sometimes required if vision results aren’t satisfactory or complications occur (up to 10%).
Remember, a major advantage of Intacs is their reversibility. Segments can be removed safely, often returning your cornea close to its original state. And importantly, having Intacs won't prevent you from pursuing a corneal transplant later if needed.
Costs and Insurance for Intacs Procedure
In the U.S., Intacs typically cost between $1,500 and $3,000 per eye. Many medical insurance plans cover Intacs when certain conditions are met:
- You're usually eligible if you're aged 21 or older.
- Intacs must be medically necessary (significant vision issues not corrected by glasses or lenses).
- Your cornea should be clear and thick enough (around 450 µm or more).
If you’re looking for ways to lower out-of-pocket costs, consider the following:
- Use medical insurance. Pre-authorize the procedure by clearly documenting medical necessity.
- Flexible Spending Accounts (FSA) or Health Savings Accounts (HSA). Pay with pre-tax dollars to save significantly.
- Payment plans. Many clinics offer interest-free financing options.
Intacs can be life-changing, but knowing your options helps you make informed decisions. If you're considering Intacs, consult with a keratoconus specialist who can thoroughly assess your candidacy and discuss realistic outcomes.
Use VisionCenter’s "Find an Eye Doctor" tool or check the American Academy of Ophthalmology (AAO) directory. Don't forget to download your consultation checklist to prepare the right questions and get the most from your visit.
In this article
7 sources cited
Updated on June 20, 2025
Updated on June 20, 2025
About Our Contributors
Vincent Ayaga is a medical researcher and seasoned content writer with a bachelor's degree in Medical Microbiology. Specializing in disease investigation, prevention, and control, Vincent is dedicated to raising awareness about visual problems and the latest evidence-based solutions in ophthalmology. He strongly believes in the transformative power of ophthalmic education through research to inform and educate those seeking knowledge in eye health.
Dr. Melody Huang is an optometrist and freelance health writer with a passion for educating people about eye health. With her unique blend of clinical expertise and writing skills, Dr. Huang seeks to guide individuals towards healthier and happier lives. Her interests extend to Eastern medicine and integrative healthcare approaches. Outside of work, she enjoys exploring new skincare products, experimenting with food recipes, and spending time with her adopted cats.

