Updated on October 8, 2024
What to Know About Keratitis


Vision Center is funded by our readers. We may earn commissions if you purchase something via one of our links.
Keratitis is a prevalent eye condition that can range from mild to severe. Understanding the different types of keratitis, their causes, and effective treatments is crucial for maintaining eye health. In this article, we’ll discuss keratitis’ causes, symptoms, and treatment options.
What is Keratitis?
Keratitis is inflammation of the cornea (the clear outer layer of the eye). It can be mild, moderate, or severe. It may involve one (unilateral) or both eyes (bilateral) and can be associated with inflammation of other regions of the eye.
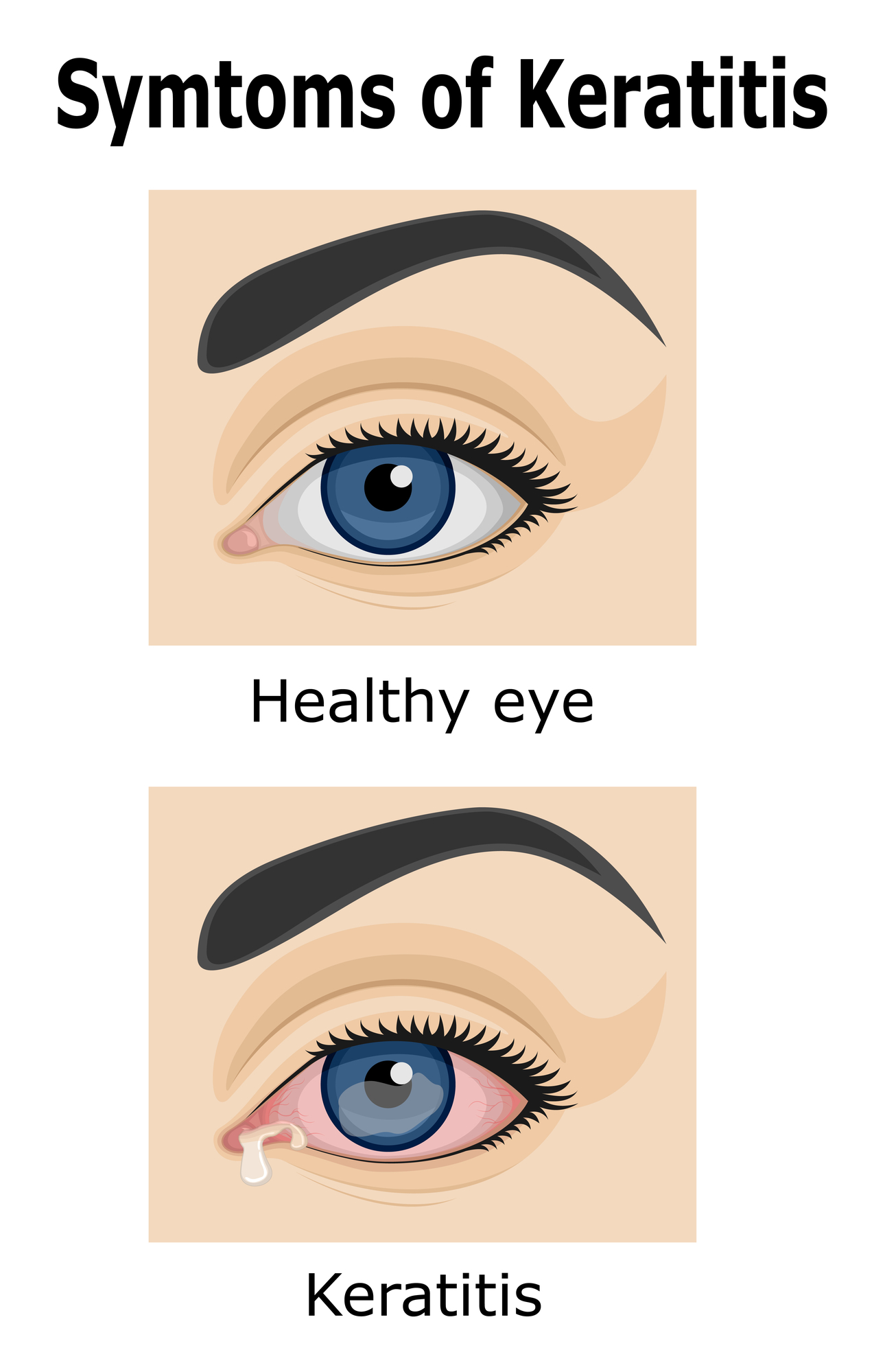
The symptoms of keratitis depend on the type a person is suffering from. These typically include:
- Eye irritation and pain
- Red eye
- Excessive tearing
- Eye discharge
- Sensitivity to light
- Blurred vision or partial blindness
- Inability to open the eyes
If you notice any of these symptoms, seek medical attention. If left untreated, keratitis can worsen over time.
Types of Keratitis and What Causes Them
Keratitis is divided into two main types: infectious keratitis (microbial keratitis) and noninfectious keratitis. Infectious keratitis is caused by bacteria, fungi, viruses, or parasites.
On the other hand, noninfectious keratitis is caused by physical trauma, weak immunity, or exposure to extreme environmental elements.
Infectious Keratitis
Infectious keratitis is a leading cause of vision impairment and blindness worldwide, disproportionately impacting marginalized populations.
These are the different types of infectious keratitis:
- Bacterial keratitis. Caused by bacteria such as Pseudomonas aeruginosa and Staphylococcus aureus. Occurs due to improper or unhygienic use of contact lenses.
- Fungal keratitis. Caused by fungi like Candida species, Fusarium and Aspergillus. It occurs due to eye trauma, improper contact lens use, and underlying diseases. It’s also common in tropical and subtropical environments.
- Viral keratitis. Caused by viruses commonly triggered by stress, a weak immune system, and exposure to direct sunlight. Typically associated with viruses such as herpes simplex virus, varicella-zoster virus, and adenovirus.
- Parasitic keratitis (or Acanthamoeba keratitis). Caused by a microscopic parasite known as Acanthamoeba, commonly found in water, soil, and air. It mainly affects people who wear contacts, those with corneal trauma, or exposure to contaminated water.
Non-infectious Keratitis
Non-infectious keratitis can result from eye injuries, a weak immune system, prolonged contact use, allergens, and exposure to extreme environments. It can be identified based on the appearance or region of the affected eye.
The types of non-infectious keratitis include:
- Diffuse lamellar keratitis. Characterized by the accumulation of white blood cells and other inflammatory cells under the corneal flap created during LASIK surgery.
- Disciform keratitis. Associated with herpes simplex virus (HSV) and causes swelling in the center of the cornea.
- Epithelial keratitis. A complication following cataract surgery. It appears as tree-like or pointed lesions.
- Filamentary keratitis. This condition is associated with corneal swelling and dry eyes. It’s characterized by strands made up of epithelial cells and mucus on the surface of the cornea.
- Punctate keratitis. This type of keratitis is associated with inflammation of the upper layer of the cornea. It is common among those with dry eye syndrome.
- Ulcerative keratitis. Also known as peripheral ulcerative keratitis. Manifests as a crescent-shaped inflammatory damage to the cornea. It’s linked to autoimmune diseases, including rheumatoid arthritis and lupus.
Listen In Q&A Format
Keratitis
Vision Center Podcast
Is Keratitis Contagious?
Some forms of keratitis can be infectious but are not often transmitted to others. For example, herpes simplex (which causes cold sores) and herpes zoster viruses (which causes chickenpox) are highly contagious and often transmitted via skin contact.
After this initial infection, the virus then lives dormant in your body until reactivation, which is when keratitis may develop. The likelihood of passing herpes keratitis onto someone else is low, but you should still practice good hygiene, such as washing your hands often.
However, keratitis caused by non-infectious elements such as eye injury may not be contagious unless an infection develops. This condition can progress rapidly. If you suspect keratitis or have a problem with your eye, seek immediate medical advice.
How is Keratitis Treated?
If you get keratitis as a result of an injury, it will usually go away on its own as your eye recovers. Treatment for keratitis depends on the cause. Common treatment options for keratitis include:
- Topical antibiotics for bacterial infections and injuries
- Antifungals such as oral voriconazole for fungal keratitis
- Antivirals such as trifluridine (USA) and Ganciclovir (Europe) for viral keratitis
- Biocides such as chlorhexidine, biguanides, and phosphocholine for parasitic keratitis
Keratitis is typically easy to treat and resolves quickly. However, if the infection spreads beyond the surface of your cornea, it may leave scars that impair your eyesight or possibly cause blindness.
In addition, not all types of keratitis respond well to treatment. For example, Acanthamoeba keratitis (caused by a parasite) can be difficult to treat and resistant to medications.
Viral medications may also fail to fully eliminate the virus in viral keratitis. If the infection persists, your doctor may need to conduct further eye examinations and implement advanced treatment options.
When Should You See a Doctor?
You should contact your doctor immediately if you experience redness, eye pain, blurry vision, or any of the symptoms mentioned before. Getting treatment early can improve your chances of recovering from keratitis quickly.
Leaving keratitis untreated can result in severe eye damage and long-term conditions such as:
- Scars on the cornea
- Long-term inflammation
- Corneal ulcers (sores on the cornea)
- Recurring infections
- Glaucoma (in rare cases)
- Vision loss
Can You Prevent Keratitis?
Yes, there are ways to prevent keratitis. Here are some tips that can help you do that:
- If you’re using contacts, follow the care regimen prescribed by your doctor.
- Always wash your hands thoroughly before touching your lenses.
- Replace your contact lenses as per your doctor’s advice.
- Avoid sleeping with your contact lenses unless your optometrist recommends it.
- Avoid swimming in your contact lenses.
- Use daily wear contacts
- Avoid touching your eyes if you have a sore or herpes blister.
- Only use doctor-prescribed eye drops.
While keratitis can be a bothersome condition, it is often treatable with appropriate medical intervention. Remember, early diagnosis and treatment are key to preventing long-term complications and preserving your vision.
In this article
6 sources cited
Updated on October 8, 2024
Updated on October 8, 2024
About Our Contributors
Vincent Ayaga is a medical researcher and seasoned content writer with a bachelor's degree in Medical Microbiology. Specializing in disease investigation, prevention, and control, Vincent is dedicated to raising awareness about visual problems and the latest evidence-based solutions in ophthalmology. He strongly believes in the transformative power of ophthalmic education through research to inform and educate those seeking knowledge in eye health.
Dr. Melody Huang is an optometrist and freelance health writer with a passion for educating people about eye health. With her unique blend of clinical expertise and writing skills, Dr. Huang seeks to guide individuals towards healthier and happier lives. Her interests extend to Eastern medicine and integrative healthcare approaches. Outside of work, she enjoys exploring new skincare products, experimenting with food recipes, and spending time with her adopted cats.

