Updated on October 21, 2024
Retinoschisis (Separated Retina)


Vision Center is funded by our readers. We may earn commissions if you purchase something via one of our links.
What is Retinoschisis?
Retinoschisis is an eye condition that causes the eye’s retina to split into two layers. Retino- refers to the retina, while -schisis refers to split. It affects both young and old, males and females.
While retinoschisis is a commonly used name, eye doctors may also refer to it as:
- Congenital retinal cyst
- Congenital vascular veils in the retina
- Giant cyst of the retina
- Vitreoretinal dystrophy
What Causes Retinoschisis?
Retinoschisis has two primary causes: genetics and degeneration.
Genetics
Retinoschisis can occur in males with a mutation or abnormal gene on the X chromosome. While females can be carriers of the mutation, it's not common for them to develop this eye disorder.
One of the two X chromosomes in females is inactivated (usually that with the mutation). As a result, there is no consequential clinical manifestation. Males with X-linked disorders like retinoschisis will pass the abnormal gene to all of their daughters.
Degeneration
It's uncommon to find this eye disorder among people younger than 40. Degenerative retinoschisis often occurs in people in their 50s, 60s, or 80s.
Signs and Symptoms of Retinoschisis
A central database called the Human Phenotype Ontology (HPO) provides a detailed and up-to-date list of symptoms related to retinoschisis.
According to the HPO, approximately 80 to 90% of people with juvenile retinoschisis will have:2
- Abnormal eye movement
- Abnormal vision (a decline in foveal or peripheral vision)
- Cataracts (clouding of the lens of the eye)
- Glaucoma (an ocular disease in which the optic nerve is damaged)
According to the HPO, approximately 30 to 79% of people with juvenile retinoschisis will have:2
- Macular atrophy (deterioration of the macula, which is the central part of the retina call)
- Retinal pigment epithelial atrophy (weakening of the pigment tissue that lines the retina)
How Serious is a Split Retina?
A split retina is a serious condition.
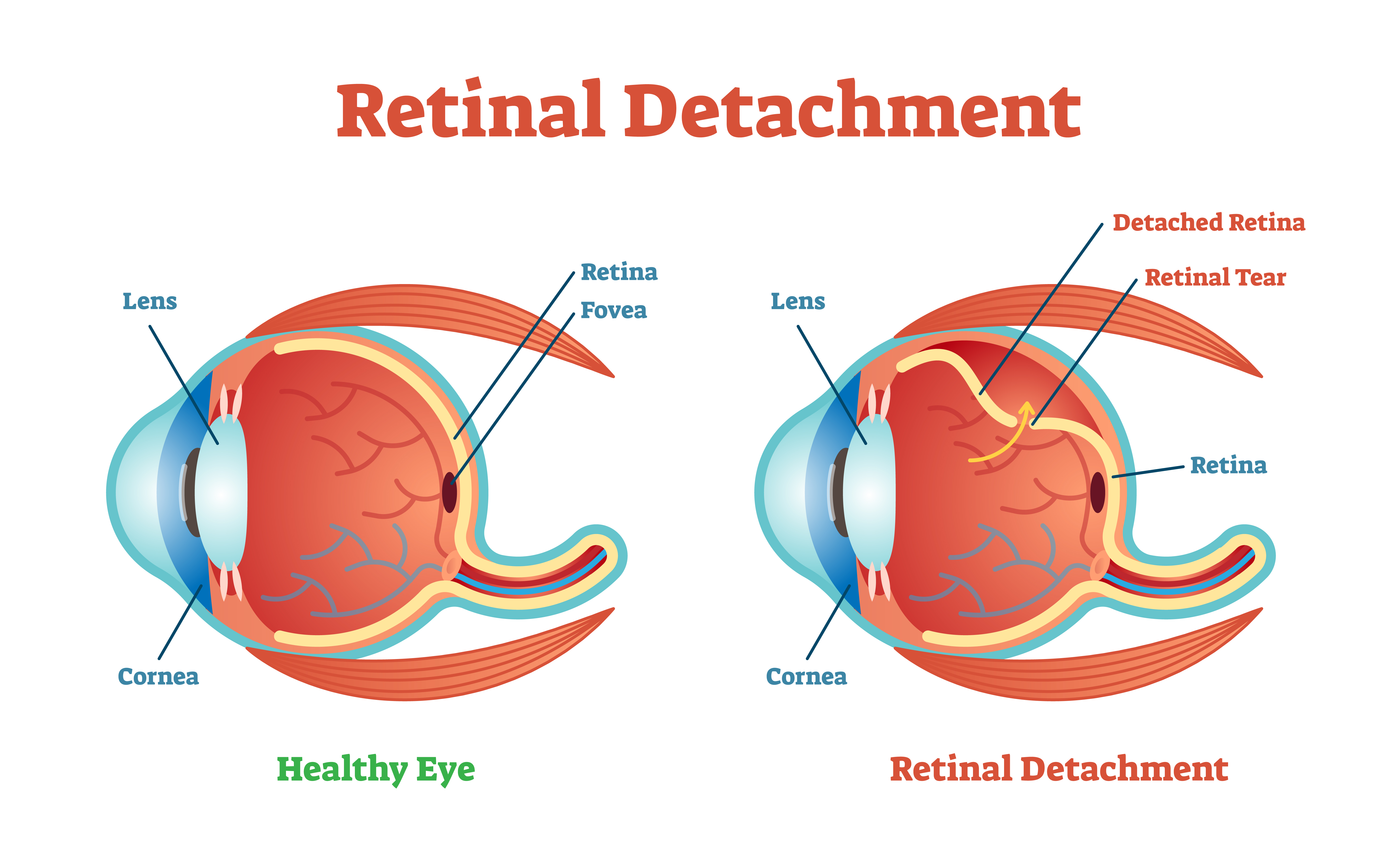
It's not common for retinoschisis to progress or result in retinal detachment. However, if there is disease progression, symptoms may appear before the loss of central vision, including:
- Flashing lights
- Loss of peripheral vision
- Floaters
Affected people should visit their local eye clinic at least once a year to make sure the eye disorder remains stable.
Potential Complications of Retinoschisis
Retinoschisis isn't something that should be left untreated. The condition presents potential complications.
Vision Loss in Retinoschisis
Retina splitting can cause slow vision loss in one of the following:
Center of Vision (Fovea)
A person with impaired central vision can have visual acuity (sharpness) between 20/30 and 20/200. The decreased vision happens because of tiny cysts (sac-like blisters).
They form between the separated layers of the retina and damaged nerve tissue. When this occurs, glasses or contact lenses won't be able to improve visual acuity.
Peripheral Vision
A person with retinoschisis can lose some peripheral vision. This is if the inner layer of nerve cells breaks off from the outer layer of cells.
Is Retinoschisis Progressive?
In cases of senile retinoschisis, the eye disorder rarely progresses. For juvenile retinoschisis, vision often decreases at a young age. It becomes stable during early or mid-adulthood.
It's also common for people with juvenile retinoschisis to experience another decline in vision in their 50s or 60s.
How is Retinoschisis Diagnosed?
An eye care specialist will use different diagnostic approaches for retinoschisis, including:
- Optical coherence tomography (OCT). This test uses light waves to create images of the retina
- An electroretinogram (ERG). This test measures light-stimulated electrical impulses, which determine if there’s an impairment of retinal functioning
- Ultrasonography or ultrasound. This diagnostic tool can help view abnormalities if the eye has suffered a hemorrhage
Retinoschisis Treatment
There is no cure for retinoschisis, but you can take steps to protect your vision and prevent further damage. Here are ways you can manage the condition:
- Carbonic anhydrase inhibitors. This is a type of medication to help reduce cystic spaces. It’s recommended for those with juvenile retinoschisis
- Laser or cryotherapy (cold). This is an option for those experiencing bleeding within the eyeball. It will cut off the damaged retinal area
- Genetic counseling. This option may be worth considering for families of children with juvenile retinoschisis
People with senile retinoschisis don't usually need medical treatments. It's recommended to have annual eye exams to make sure the condition remains stable.
If you experience any vision changes, it's essential to seek medical attention as soon as possible.
Listen In Q&A Format
Retinoschisis: Separated Retina
Vision Center Podcast
4 Types of Retinoschisis
Eye doctors can detect specific clinical characteristics and health conditions related to retinoschisis. Different diagnostic tools are available. Some people with retinoschisis may be eligible for specific treatments.
The types of retinoschisis include:
1. Degenerative Retinoschisis
Health professionals may use the following terms to describe senile retinoschisis:
- Degenerative retinoschisis
- Acquired retinoschisis
This eye disorder affects both males and females in middle age. But it can also appear in some people at an earlier age. A person with degenerative retinoschisis may be asymptomatic.
Often, the diagnosis is incidental. It can occur after a referral to a retinal specialist under the presumptive diagnosis of retinal detachment. This is when there's loosening of a thin layer in the retina.
In typical cases of degenerative retinoschisis, inner retinal layers have a shallow rise. Disease progression is not typical. Many times, it involves the peripheral retina. Many people with this eye disorder do well and only require a follow-up.
2. X-linked Juvenile Retinoschisis (XLRS)
Juvenile retinoschisis (or congenital X-linked retinoschisis) is a hereditary eye disorder. It affects males. It's a genetic disease of the retina that almost always affects both eyes (bilateral).
When a person develops juvenile retinoschisis, vision worsens early in life. Visual acuity may be between 20/60 and 20/120.
Juvenile retinoschisis is estimated to impact one in 5,000 to 25,000 people.4 It's one of the leading causes of juvenile macular degeneration.
3. Tractional Retinoschisis
Tractional retinoschisis is a disorder often confused with tractional retinal detachment.
Some unique characteristics define tractional retinoschisis. These include:
- People with this condition will have a tractional (pulled or drawn up) elevation of the retina
- The layer will be transparent
- Pigment lines will not develop
- Holes can be present in the raised retina; no change in its contour will occur
People with diabetes or sickle cell disease may have an increased risk of tractional retinoschisis.
4. Exudative Retinoschisis
This is a subclassification of retinoschisis. A lipid (fat) is in color fundus photography and clinical examination.
Color fundus (retinal) photography uses a camera to collect color images of the condition of the eye’s interior surface.
Summary
Retinoschisis is an eye disorder that affects the retina, caused by genetics or degeneration. It can cause slow vision loss and other vision problems.
While there is no cure for retinoschisis, there are several ways to manage the condition. Talk to your eye doctor to determine how to protect your vision and prevent further damage.
In this article
6 sources cited
Updated on October 21, 2024
Updated on October 21, 2024
About Our Contributors
Mara Sugue, with a B.A. in Social Sciences, is a dedicated web content writer for Vision Center. She is committed to making eye health research accessible and understandable to people from diverse backgrounds and educational levels. Her writing aims to bridge the gap between complex vision health topics and readers' needs for clear, factual information.
Dr. Melody Huang is an optometrist and freelance health writer with a passion for educating people about eye health. With her unique blend of clinical expertise and writing skills, Dr. Huang seeks to guide individuals towards healthier and happier lives. Her interests extend to Eastern medicine and integrative healthcare approaches. Outside of work, she enjoys exploring new skincare products, experimenting with food recipes, and spending time with her adopted cats.

