Updated on March 25, 2025
What is the Prevalence of Ocular Surface Diseases?


Vision Center is funded by our readers. We may earn commissions if you purchase something via one of our links.
Ocular surface disease refers to a spectrum of chronic eye conditions, most commonly dry eye disease (DED), blepharitis, and meibomian gland dysfunction (MGD). These disorders affect the tear film, eyelids, and corneal surfaces, often causing discomfort, visual fluctuations, and a major impact on daily activities.
Although rarely sight-threatening in their early stages, ocular surface diseases can significantly reduce quality of life and generate substantial healthcare costs.
In recent years, the aging population, increasing screen use, and heightened awareness of eye health have thrust ocular surface disorders into the public eye. Understanding how often these conditions occur, who is most at risk, and how they influence healthcare delivery is critical for developing effective, evidence-based interventions.
Noteworthy Statistics
- Prevalence in U.S. Adults: Dry eye disease is diagnosed in roughly 6.8% of the adult population in the United States (approximately 16 million people), with some estimates suggesting up to 9% when accounting for undiagnosed cases.
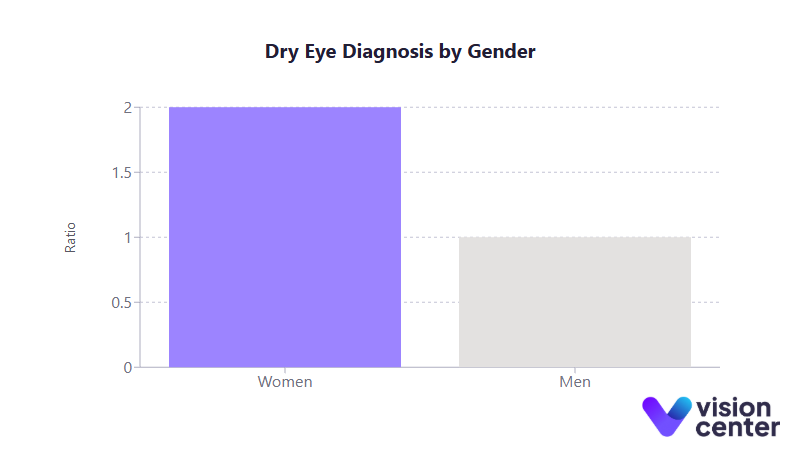
- Gender Disparity: Women are nearly twice as likely as men to be diagnosed with dry eye, a difference often attributed to hormonal factors and postmenopausal changes.
- Blepharitis in Eye Clinics: Clinical practice data indicates that 37 to 47% of patients visiting eye care providers show signs of blepharitis, illustrating how pervasive eyelid inflammation is.
- Economic Burden: Dry eye disease alone may cost the U.S. an estimated $55 billion per year in combined direct medical expenses and productivity losses.
Understanding the Prevalence of Ocular Surface Disease
Ocular surface disease is an umbrella term for conditions that compromise the integrity and function of the eye’s outermost structures. The most recognized is dry eye disease, in which tears either evaporate too quickly or are produced in insufficient amounts.
Blepharitis, an inflammation of the eyelids, and meibomian gland dysfunction, where lipid secretion in the tear film is disrupted, are also key contributors. These disorders often overlap: for example, MGD commonly coexists with dry eye.
Why This Data Matters
Statistical evidence about prevalence and demographic patterns helps clinicians, public health officials, and patients recognize the scope of ocular surface disease. By pinpointing the populations most at risk and the factors that exacerbate these conditions, stakeholders can design targeted screening programs, allocate research funding effectively, and implement early interventions that reduce the overall burden on both individuals and the healthcare system.
- Age-Related Surge: Numerous large-scale studies indicate that older adults make up the majority of patients experiencing moderate to severe ocular surface complaints. One survey found that while only 2 to 3% of adults aged 18 to 34 report dry eye symptoms, that figure jumps to 18 to 19% for those over 75.
- Gender Discrepancies: Women have almost double the risk of dry eye compared to men. Among seniors over 75, over 22% of women suffer from chronic dry eye, contrasted with about 13% of men.
- Racial and Geographic Variation: Although the differences by race are less dramatic than those by age or gender, certain studies show slightly higher rates in some ethnic groups. Geographically, urban regions with poor air quality can see notably elevated prevalence, sometimes 3 to 4 times higher than less-polluted areas.
Risk Factors in Detail
- Hormonal Influences: Shifts in estrogen and androgen levels, particularly after menopause, help explain the more frequent presentation in women.
- Systemic Conditions: Autoimmune diseases (such as Sjögren’s syndrome and rheumatoid arthritis) drastically increase susceptibility to ocular surface disorders, as does diabetes mellitus.
- Medication Side Effects: Many antidepressants, antihistamines, and blood pressure medications reduce tear production or alter tear chemistry.
- Lifestyle and Environment: Chronic screen use diminishes blink rates, while environments with low humidity or high pollution can significantly aggravate symptoms.
- Coexisting Ocular Issues: Blepharitis, demodex infestations, and post-surgical corneal nerve changes (e.g., after LASIK) often trigger or worsen dry eye.
Trends in Treatment and Management
Why This Data Matters
Treatment approaches have evolved dramatically over the past decade, moving from merely masking symptoms to actively addressing underlying inflammation, meibomian gland function, and individual risk factors.
Data on efficacy and patient outcomes informs best practices, ensures cost-effective resource allocation, and helps patients understand their prognosis.
First-Line Therapies and Beyond
- Lubricating Eye Drops: Artificial tears remain the cornerstone for mild dry eye. These products have diversified in recent years, incorporating oils, polymers, and osmoprotectants to improve tear film stability. Nonetheless, relief is often temporary, necessitating frequent use.
- Eyelid Hygiene: For blepharitis and MGD, warm compresses and lid scrubs are essential initial steps. Adherence to proper hygiene can substantially reduce eyelid inflammation and help restore healthy tear film.
- Prescription Anti-Inflammatories:
- Cyclosporine Eye Drops: Over the years, around half of chronic dry eye patients have tried cyclosporine, which targets inflammation at the ocular surface. Although many experience measurable symptom relief, a subset do not respond sufficiently.
- Lifitegrast Eye Drops: Approved more recently, lifitegrast often demonstrates faster improvement of dryness symptoms, showing benefits as early as two weeks in clinical trials.
- Corticosteroids: Used in short bursts to calm disease flares, these drops can rapidly reduce inflammation but carry risks if used long-term (elevated eye pressure, cataracts).
- Autologous Serum Tears: Derived from a patient’s own blood, serum eye drops are particularly beneficial in severe cases where other treatments fail, offering vital growth factors that help heal the cornea. Access, however, can be limited by cost and specialized lab requirements.
Advanced Procedures and Devices
- Punctal Plugs: By blocking tear drainage channels, these plugs allow natural tears to stay on the eye surface longer. They can be life-changing for those with significantly decreased tear production.
- Thermal Pulsation (e.g., LipiFlow): Applying heat and gentle pressure to the eyelids expresses clogged meibomian glands. Clinical data suggests up to 79% of patients see symptom improvement within a month, with effects often lasting up to a year.
- Intense Pulsed Light (IPL) Therapy: Originally used in dermatology, IPL is now employed to manage MGD. Reports show that up to 80 to 90% of treated patients experience substantial relief.
- Lid Debridement Tools: Micro-sponge devices and targeted hygiene regimens remove debris and mites from eyelid margins, easing stubborn blepharitis.
- Scleral Lenses: For severe ocular surface disease, specially fitted contact lenses create a fluid reservoir over the cornea, bringing lasting comfort and clearer vision where conventional therapies fall short.
Growing Adoption of Combination Therapy
A major shift over the last decade has been the recognition that single treatments rarely suffice. Multi-modal plans (combining artificial tears, prescription drops, and in-office procedures) often yield significantly better symptom control.
While initial costs can be higher, studies suggest that comprehensive therapy decreases complications and overall healthcare spending in the long run. Nonetheless, cost and insurance coverage remain substantial barriers for many.
Patient Impact and Cost Burden
Why This Data Matters
Beyond prevalence and treatments, understanding the personal and societal impact of ocular surface disease underscores the urgency of improving screening and care. This includes direct medical costs, workplace productivity losses, and the often underappreciated emotional toll chronic eye discomfort can impose.
Economic Costs
- High Direct Expenditures: Doctor visits, advanced treatments like IPL, and continuous use of artificial tears can push yearly patient expenses toward $780 or more.
- Productivity Losses: Businesses shoulder indirect costs, as employees with persistent ocular irritation may need more breaks, reduced screen time, and sick days. Estimates place the overall annual productivity hit above $50 billion nationally.
- Total Annual Burden: When direct and indirect costs are combined, dry eye disease can cost the United States around $55 billion per year, making it one of the most financially consequential eye conditions.
Quality of Life
Daily tasks like driving, reading, and working on digital devices become arduous when dryness, stinging, and blurry vision persist. Surveys reveal that moderate to severe ocular surface disease can lower quality-of-life scores to levels akin to other chronic systemic conditions.
Many patients report anxiety, irritability, or social withdrawal as they struggle to manage constant discomfort. Improvements in therapy do help, but full symptom resolution remains elusive for a notable portion of those affected.
Environmental Challenges
Air pollution, extreme wind, and very low humidity settings are frequent triggers for symptom flare-ups. In major urban centers with higher pollution, dry eye rates can run 3 to 4 times higher than in cleaner rural environments.
Meanwhile, heated or air-conditioned indoor spaces reduce ambient moisture, aggravating dryness. These insights highlight the benefits of consistent lid care, protective eyewear, and the potential role of humidifiers in mitigating symptom severity.
Healthcare Delivery, Access, and Long-Term Outcomes
Why This Data Matters
From demographic patterns in clinic visits to disparities in insurance coverage, the way healthcare is delivered can influence both how quickly patients receive a diagnosis and the treatment methods available to them. In turn, early and appropriate management often forestalls the most serious complications.
Access and Demographics
- Older, Female Population Domination: Postmenopausal women continue to represent a large share of those seeking help for ocular surface disease, aligning with higher prevalence. However, clinics report an uptick in younger individuals presenting with dryness linked to computer use.
- Insurance Gaps: Studies show that insured individuals are diagnosed with dry eye at roughly double the rate of those without insurance, a discrepancy suggesting that many patients may be underdiagnosed or unable to afford advanced therapies.
- Geographic Differences: Cities with heavier pollution (e.g., Los Angeles, Chicago) see more frequent clinic visits for dry eye. Dry, high-altitude states like Arizona and Nevada also have higher risk, prompting some local practices to adopt more aggressive screening and early interventions.
Long-Term Prognosis
Ocular surface disease can progress over years if unaddressed, but better detection and multi-modal treatment now prevent many severe complications seen in the past. Despite these improvements:
- Progression and Flare-Ups: Even well-managed patients can experience periodic disease flares due to medication changes, hormonal shifts, or environmental factors.
- Refractory Cases: Those with severe autoimmune diseases or underlying conditions might only achieve partial relief. Scleral lenses, autologous serum drops, or more invasive measures remain essential options for late-stage disease.
- Future Directions: Ongoing research explores emerging therapies, such as new tear secretagogues and novel device-based treatments, and emphasizes personalized care. The trend toward consistent, lifelong management strategies echoes protocols used for other chronic health conditions (e.g., diabetes or hypertension).
Over the last decade, the conversation around ocular surface disease has evolved from viewing it as a minor nuisance to recognizing it as a significant public health concern. These conditions remain widespread, affecting tens of millions of Americans, but the growing toolkit of targeted therapies and procedural interventions offers hope for better symptom control and prevention of disease progression.
Early intervention is key now more than ever. As awareness expands across primary care and ophthalmic specialties alike, the long-term trajectory for many patients has improved, though challenges in cost, access, and refractory cases persist.
In looking ahead, experts anticipate a continued focus on combination treatments, advanced imaging to track meibomian gland health, and possibly new pharmacological breakthroughs. In the bigger picture, the data-driven insights gleaned over the past decade point strongly toward a future in which ocular surface disease is addressed in a manner befitting its true impact: proactively, comprehensively, and with patient-centered care at the forefront.
Thanks to the proliferation of research and the diversity of treatments now available, more patients than ever are finding the relief they need to preserve both their vision and overall quality of life.
In this article
4 sources cited
Updated on March 25, 2025
Updated on March 25, 2025
About Our Contributors
Mara Sugue, with a B.A. in Social Sciences, is a dedicated web content writer for Vision Center. She is committed to making eye health research accessible and understandable to people from diverse backgrounds and educational levels. Her writing aims to bridge the gap between complex vision health topics and readers' needs for clear, factual information.
Dr. Melody Huang is an optometrist and freelance health writer with a passion for educating people about eye health. With her unique blend of clinical expertise and writing skills, Dr. Huang seeks to guide individuals towards healthier and happier lives. Her interests extend to Eastern medicine and integrative healthcare approaches. Outside of work, she enjoys exploring new skincare products, experimenting with food recipes, and spending time with her adopted cats.

