Updated on March 25, 2025
Glaucoma Risk Factors Statistics: What You Need to Know


Vision Center is funded by our readers. We may earn commissions if you purchase something via one of our links.
Glaucoma is a leading cause of irreversible blindness and often shows no early symptoms, which makes it a silent threat to vision health. Understanding the statistical landscape of glaucoma, from its risk factors and demographic patterns to its broader population impact, can play a vital role in advancing early detection and effective prevention strategies.
Glaucoma primarily affects the optic nerve and can lead to progressive, permanent vision loss if not diagnosed and treated in time. While it often goes undetected until significant damage has occurred, extensive research has identified several risk indicators, most notably age, ethnicity, and family history.
This data-driven exploration presents a comprehensive look at the prevalence of glaucoma, the demographic disparities observed, and the economic burden associated with this complex eye condition.
Key Statistics at a Glance
- Age-Linked Prevalence: Risk sharply rises after age 60, with older adults facing a significantly greater likelihood of developing glaucoma.
- Undetected Cases: Approximately half of people with glaucoma in the United States are unaware they have it, indicating a substantial gap in diagnosis.
- Family History Factor: Individuals with a first-degree relative diagnosed with glaucoma may have up to a fourfold increased risk of developing the disease themselves.
- Projected Growth: By 2050, the number of Americans with glaucoma may reach 6 million, reflecting the nation’s aging population and shifting demographics.
Understanding Glaucoma: Why the Data Matters
Glaucoma’s stealthy progression and potential to cause irreversible vision loss highlight why reliable data on risk factors is crucial.
Public health experts, policymakers, and healthcare providers rely on these statistics to prioritize screening programs and allocate resources effectively. Below, we delve into the major risk factors, prevalence trends, and how these findings shape the fight against glaucoma.
Age as a Primary Risk Factor
Age has consistently been identified as one of the strongest predictors of glaucoma:
- Sharp Increase with Age
- Glaucoma prevalence remains relatively low (under 1%) in individuals younger than 40.
- By age 60, the prevalence can exceed 2 to 3% in many population groups.
- In those 80 and older, some data suggest that over 10% may develop glaucoma, underscoring the importance of regular eye examinations for seniors.
- Early vs. Late Detection
- Many older adults are not diagnosed until the moderate or advanced stages because early glaucoma rarely causes noticeable symptoms.
- Increased vigilance in routine vision screenings among adults aged 60 and above could substantially reduce instances of late-stage detection.
Ethnicity and Demographic Disparities
Glaucoma rates vary among racial and ethnic groups, indicating that certain communities face elevated risks:
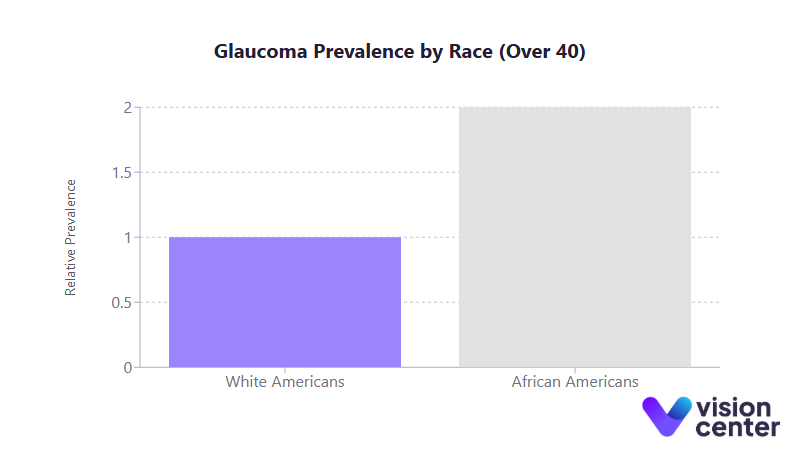
- Higher Prevalence in African American and Hispanic Populations
- African Americans over age 40 have nearly double the rates of glaucoma compared to white Americans of the same age range.
- Among older Hispanic/Latino groups, prevalence can be comparable to or even surpass that seen in African American communities.
- Research also shows that African Americans are more likely to experience vision-threatening or advanced glaucoma.
- Impact on Public Health
- These disparities lead to disproportionate rates of vision loss and blindness in specific populations.
- Targeted outreach and screening programs can help mitigate the higher rates of undiagnosed cases in these communities.
Family History and Genetics
Glaucoma does not solely occur due to genetics, but family history plays an outsize role in predicting risk:
- Increased Susceptibility
- Having a first-degree relative (parent or sibling) with glaucoma increases one’s own risk by up to three to four times.
- Genetic predisposition can be associated with certain gene mutations (like MYOC), though the disease is often polygenic.
- Screening Recommendations
- Close relatives of glaucoma patients are often urged to begin screening earlier and to do so more frequently.
- Early identification of familial patterns helps eye care professionals intervene well before significant optic nerve damage occurs.
Other Health Conditions and Lifestyle Factors
Several coexisting conditions and lifestyle choices appear to influence glaucoma risk:
- Medical Comorbidities
- Diabetes and hypertension have been linked to a higher likelihood of developing glaucoma.
- Eye conditions such as ocular hypertension (elevated eye pressure) and thin corneas can further heighten risk.
- Lifestyle Elements
- Smoking and poor cardiovascular health are sometimes associated with an increased chance of intraocular pressure spikes.
- Adopting a balanced diet and maintaining good overall health can potentially support healthier eye pressure levels.
Prevalence and Demographic Breakdowns
Detailed statistical analyses offer a window into which groups are most affected and how these patterns shift over time. Understanding these numbers is fundamental to shaping targeted interventions.
National Overview
- Overall Glaucoma Cases
- Around 3 to 4 million U.S. adults are estimated to have glaucoma, though many remain undiagnosed.
- Glaucoma accounts for roughly 9 to 12% of all cases of blindness in the United States.
- Age-Specific Distribution
- Under 40: Prevalence is typically less than 1%.
- 40 to 59: Risk starts to climb gradually, often reaching 2 to 3%.
- 60+: Prevalence can exceed 5% depending on ethnicity and overall health profile.
- Gender Variations
- Women comprise a slightly higher share of glaucoma cases, partly due to longer life expectancy.
- Among individuals 70 and older, some estimates show more female than male patients overall.
Racial Disparities in Detail
| Age Group | Glaucoma Prevalence in White Americans | Glaucoma Prevalence in African Americans | Glaucoma Prevalence in Hispanic/Latino Americans |
| 40–49 | ~0.6% | ~1.2% | ~0.5% |
| 60–69 | ~1.6% | ~5.0 to 5.7% | ~2.0 to 2.4% |
| 80+ | ~7.0 to 7.5% | ~10 to 12% | ~10% |
Why it matters: As the U.S. population diversifies, the absolute number of glaucoma cases in Hispanic/Latino Americans is expected to increase substantially. By mid-century, half of all glaucoma cases in the country may be in this group, highlighting the need for culturally tailored eye health initiatives.
Time Trends and Future Projections
- Steady Rise Due to Aging
- The 65+ population in the U.S. is growing faster than any other age segment, boosting overall glaucoma prevalence.
- Projections indicate 5 to 6 million people could be diagnosed by 2050, a sizable jump from current estimates.
- Potential Policy Implications
- Healthcare systems might see higher demand for ophthalmological services and increased costs for prevention and treatment programs.
- Early detection and cost-effective screening models could help manage future burdens.
Treatment Efficacy and Outcomes
While there is no definitive cure for glaucoma, effective management can slow or halt disease progression. The data on treatment outcomes are essential for both clinicians and patients seeking the best approach to preserve vision.
Standard Therapies: Eye Drops, Laser, and Surgery
- Eye Pressure Reduction
- Lowering intraocular pressure is the central strategy for preserving the optic nerve.
- Medications such as prostaglandin analogs can reduce eye pressure by 25 to 30% on average.
- Laser procedures and surgical interventions can provide similar or greater pressure reduction, especially in more advanced or treatment-resistant cases.
- Clinical Trial Insights
- Studies show that lowering pressure by about a quarter can reduce the rate of visual field loss significantly over several years.
- Early intervention in patients with ocular hypertension (elevated eye pressure but no existing nerve damage) has been shown to cut the risk of developing full-blown glaucoma by more than half.
Quality of Life and Long-Term Vision Preservation
- Visual Field Protection
- Approximately 90% of those who receive appropriate care can maintain functional vision throughout their lifetime.
- Nonetheless, around 10% of treated patients still experience some level of vision loss, highlighting the importance of consistent follow-up.
- Quality of Life Impact
- Glaucoma-related visual impairment can limit daily activities like driving, reading, and walking.
- Research suggests that individuals with advanced glaucoma may be at higher risk of falls and accidents, which may result in greater healthcare costs and reduced independence.
- Progress in Recent Decades
- Population-based studies indicate that the probability of going blind from glaucoma within 20 years of diagnosis has nearly halved compared to figures from the mid-20th century.
- Ongoing advancements in treatment techniques (e.g., microinvasive glaucoma surgeries) continue to improve patient outcomes.
Economic and Social Impact
Glaucoma imposes a considerable financial burden on both individuals and healthcare systems. Understanding the scope of these costs can inform policymakers and payers about where to focus prevention and care resources.
- Direct Medical Costs
- Eye drops, surgical procedures, ongoing follow-up visits, and supportive therapies contribute to annual spending in the billions of dollars nationwide.
- As more people are diagnosed, particularly older adults with complex medical needs, these costs are expected to climb.
- Indirect Costs
- Vision loss can lead to reduced productivity, early retirement, and increased dependency on caregivers.
- Families and social services often shoulder additional expenses for transportation, home modifications, or assistive devices.
- Public Health Perspective
- Glaucoma’s stealthy onset means many cases go undetected until advanced stages, significantly driving up treatment expenses and associated losses in quality of life.
- Screening interventions aimed at high-risk groups (especially older adults and certain ethnicities) can reduce long-term costs by catching the disease earlier.
Notable Prevention and Screening Initiatives
Given the high rate of undiagnosed glaucoma and the essential role of early detection, targeted programs have emerged to close the diagnosis gap:
- Community Outreach
- Mobile clinics and vision screening events in low-income and rural areas have improved access to basic eye examinations.
- Bilingual education materials and culturally competent healthcare providers help reach Hispanic/Latino and other underserved communities.
- Comprehensive Eye Exams
- Annual or biennial eye exams, particularly for people over 60 or those with a strong family history, are strongly advised.
- Eye professionals can detect subtle changes in intraocular pressure or the optic nerve, enabling earlier intervention.
- Public Awareness Campaigns
- Organizations emphasize the importance of baseline screenings by age 40, given that glaucoma can begin developing at mid-life.
- Campaigns address myths (e.g., “no symptoms means no risk”) to encourage consistent monitoring.
Why it matters: When detected early, glaucoma can often be managed effectively to prevent or significantly delay vision loss. Investments in screening and public education thus have a demonstrable return in terms of reduced healthcare costs and preserved quality of life.
Final Summary
Glaucoma stands out for its silent progression and potentially devastating effects on vision health. The data shows that older adults, especially those over 60, and specific ethnic groups like African Americans and Hispanics are disproportionately affected. Family history remains a key predictor of risk, underscoring the role of genetics in disease onset.
Despite rising prevalence and demographic shifts, modern treatment options are highly effective at slowing disease progression. Early detection is crucial, however, and the significant number of undiagnosed cases highlights a critical need for more accessible screening programs.
Continued advancements in treatment and screening programs promise to mitigate vision loss and improve the quality of life for those at risk. In particular, investing in early detection initiatives could lead to substantial gains, both in preserving vision and lowering healthcare costs.
The statistics surrounding glaucoma underscore an important reality: with timely intervention, countless individuals can maintain healthy, independent lives despite a diagnosis of this complex eye condition.
In this article
4 sources cited
Updated on March 25, 2025
Updated on March 25, 2025
About Our Contributors
Mara Sugue, with a B.A. in Social Sciences, is a dedicated web content writer for Vision Center. She is committed to making eye health research accessible and understandable to people from diverse backgrounds and educational levels. Her writing aims to bridge the gap between complex vision health topics and readers' needs for clear, factual information.
Dr. Melody Huang is an optometrist and freelance health writer with a passion for educating people about eye health. With her unique blend of clinical expertise and writing skills, Dr. Huang seeks to guide individuals towards healthier and happier lives. Her interests extend to Eastern medicine and integrative healthcare approaches. Outside of work, she enjoys exploring new skincare products, experimenting with food recipes, and spending time with her adopted cats.

