Updated on February 20, 2024
Gonococcal Conjunctivitis (Gonorrhea in the Eye)


Vision Center is funded by our readers. We may earn commissions if you purchase something via one of our links.
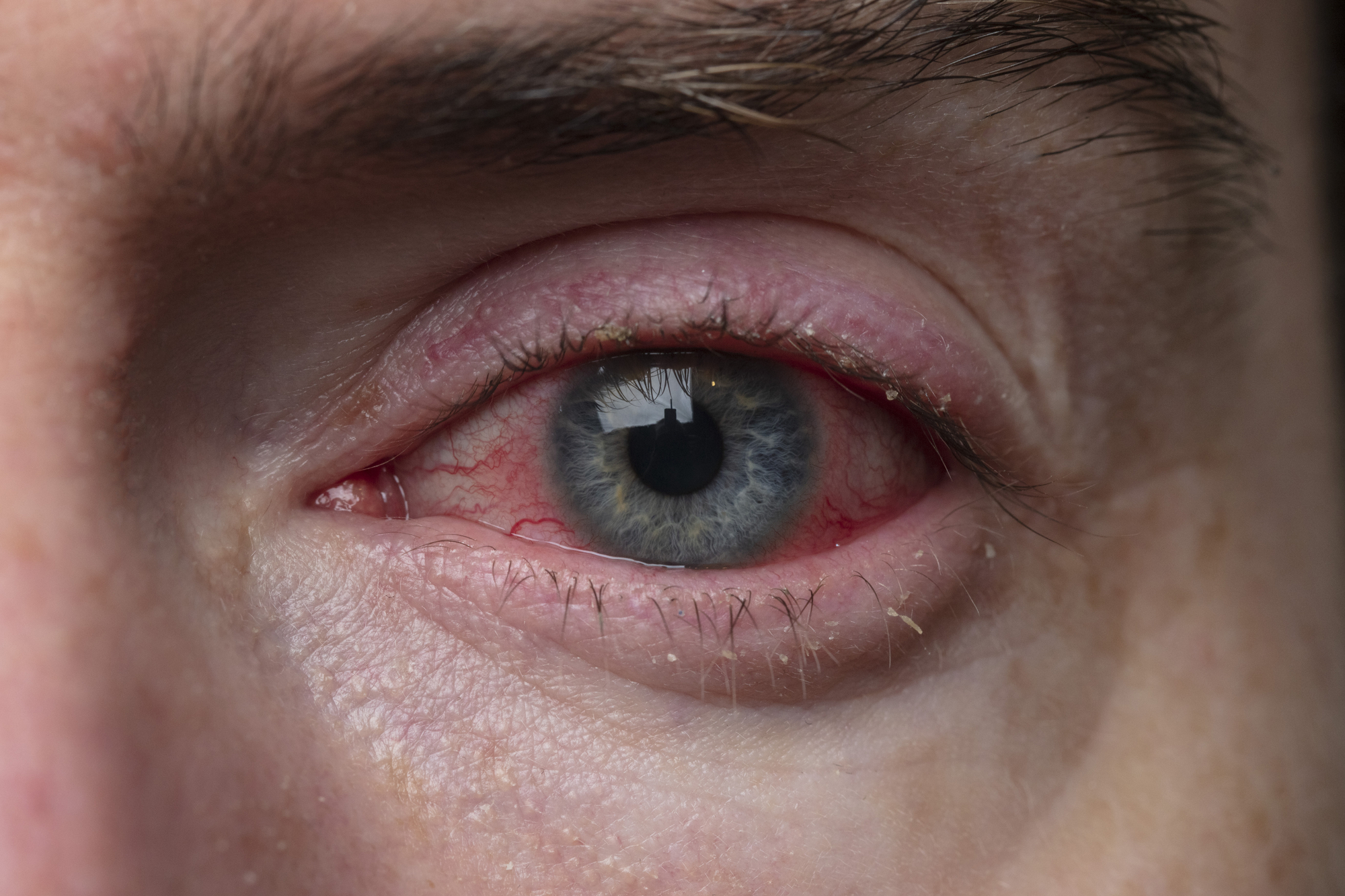
Symptoms of Gonorrhea Conjunctivitis
The infection has an incubation period of 3 to 19 days. This means someone may not show signs or symptoms until at least 3 days after contracting the infection.
Infection symptoms include:
- Chemosis. When the conjunctiva (the clear tissue covering your eyeball and eyelids) is swollen.
- Purulent discharge. A stringy, mucus-like white or yellow substance may come out of the eyes.
- Eyelid swelling. Eyelids may become puffy and swollen as a result of contracting GC.
- Conjunctival infection. When the whites of your eyes turn red.
- Corneal ulceration. In severe cases, the cornea (the clear outer layer of the eye) may develop an ulcer due to the infection.
Someone with any of these symptoms should promptly consult an eye doctor. If symptoms are severe or reappear, tested lab samples can confirm the diagnosis.


Gonococcal Conjunctivitis Diagnosis
Doctors can diagnose GC by taking a sample from the eye and viewing it under a microscope. The sample will show the presence of gonorrhea bacteria in the eye.
If you have symptoms of GC, your doctor may take a swab from your eye. Then, they’ll send it to a lab for testing or look for Neisseria gonorrhoeae bacteria in a culture.
Other tests that can help detect N. gonorrhoeae include:
- Gram stain. A Gram stain is a type of lab test that reveals the shape and color of bacteria under a microscope. It also shows whether the bacteria are gram-positive or gram-negative.
- Screening for other STIs. Your doctor may also screen for other STIs to rule out other infections with similar symptoms.
- Genital and throat swabs. People with GC risk factors may also be asked for swab samples from the throat or genitals.
Preventing Gonococcal Conjunctivitis
Gonococcal conjunctivitis risk factors include those that can increase the risk of infection. Fortunately, there are different ways to prevent the disease.
You can prevent the transmission of gonococcal conjunctivitis by:
- Practicing safe sex. Using condoms every time you have sexual contact (especially with strangers) can protect against the spread of gonorrhea.
- Maintain contact lens hygiene. Bacteria can linger on eyewear like contact lenses, so practice good hand hygiene and proper contact lens storage.
- Maintain a healthy immune system. A compromised immune system makes you more prone to infections, so maintain a healthy lifestyle.
- Avoid sharing personal items. Don't share eyeliner, mascara, or any other personal items or products with others.
How to Treat and Manage Gonococcal Conjunctivitis
GC treatment and management depends on the condition’s severity:
Antibiotic Therapy
GC requires prompt antibiotic therapy. The type of antibiotic(s) needed depends on whether the person is treated inpatient or outpatient.
Healthcare providers can administer antibiotic eye drops to prevent GC in newborns.
Other Medication
High-risk cases require inpatient treatment. Inpatient treatment medication include:
- Cefoxitin
- Ceftriaxone
- Cefotaxime
- Spectinomycin
Outpatient antibiotics include:
- Ceftriaxone
- Azithromycin
Complications of Gonococcal Conjunctivitis
If left untreated, corneal perforation, blindness, and other severe complications can occur. Complications may include:
- Limited eye movement. GC can cause severe swelling that may limit your eye movement.
- Misdiagnosis risks. GC symptoms can be misdiagnosed as other eye problems if not treated promptly, leading to improper treatment.
- Chronic eye problems. Untreated GC may lead to chronic eye problems that impact the eye’s overall health and facilitate complications in the long run.
- Potential for cornea damage. Corneal damage and scarring are possible and may cause irreversible damage.
How to Maintain Good Eye Health
Prioritize maintaining good eye health when recovering from GC. This involves:
Try Warm Compresses
Washing the eyelid and applying warm, wet compresses can help keep the eye area clean. Gently wash the eye area with a mild cleanser and warm water. This can soothe discomfort, reduce swelling, and remove any discharge.
Use Hand Sanitizers
Hand sanitizers are a great help when you can't wash your hands. Always carry a small bottle of alcohol-based hand sanitizer to use to reduce the risk of transferring bacteria to your eyes.
Avoid Swimming in Pools
Avoid swimming in public pools, especially when you’re recovering from GC. Pool water may contain chlorine and other chemicals that irritate eyes. Swimming in public pools may also increase your exposure to various microorganisms and bacteria that can worsen eye infections.
Avoid Touching Your Eyes
Another way to maintain good eye health while recovering from GC is to avoid contact between the infected and healthy eye. The infection can spread easily if you touch your eyes with dirty or contaminated hands.
Consult Your Eye Doctor
Consult a medical care provider for additional tips. Your eye doctor can provide advice on how to keep your eyes healthy and protect them from further infection.
GC in Babies
Babies can also contract GC through contact with the birth canal during delivery. Conjunctival infection in newborns is called neonatal conjunctivitis.
It’s also possible for babies to contract neonatal conjunctivitis if contaminated fingers touch their eyes.
Symptoms of gonococcal conjunctivitis in babies include:
- Eye redness
- Eye discharge
- Excessive tearing
- Eyelid swelling
Summary
Gonococcal conjunctivitis (GC) is a type of bacterial conjunctivitis. It is commonly associated with the STD gonorrhea. If you experience this condition, consult an eye doctor immediately. They'll assess your condition to determine the best treatment.
In this article
6 sources cited
Updated on February 20, 2024
Updated on February 20, 2024
About Our Contributors
Anthony Armenta, a graduate in International Relations from the University of California, Irvine, has dedicated the past 5 years to freelance health content writing and medical editing in Barcelona. Working with public hospitals, he covers various medical specialties, including infectious diseases and pneumology. Anthony's commitment to creating fact-driven, health-related content is driven by his belief in the power of information to empower individuals to improve their health, including in areas like vision care.
Dr. Melody Huang is an optometrist and freelance health writer with a passion for educating people about eye health. With her unique blend of clinical expertise and writing skills, Dr. Huang seeks to guide individuals towards healthier and happier lives. Her interests extend to Eastern medicine and integrative healthcare approaches. Outside of work, she enjoys exploring new skincare products, experimenting with food recipes, and spending time with her adopted cats.

