Updated on February 20, 2024
Understanding Corneal Ectasia: Types, Symptoms, and More

Vision Center is funded by our readers. We may earn commissions if you purchase something via one of our links.
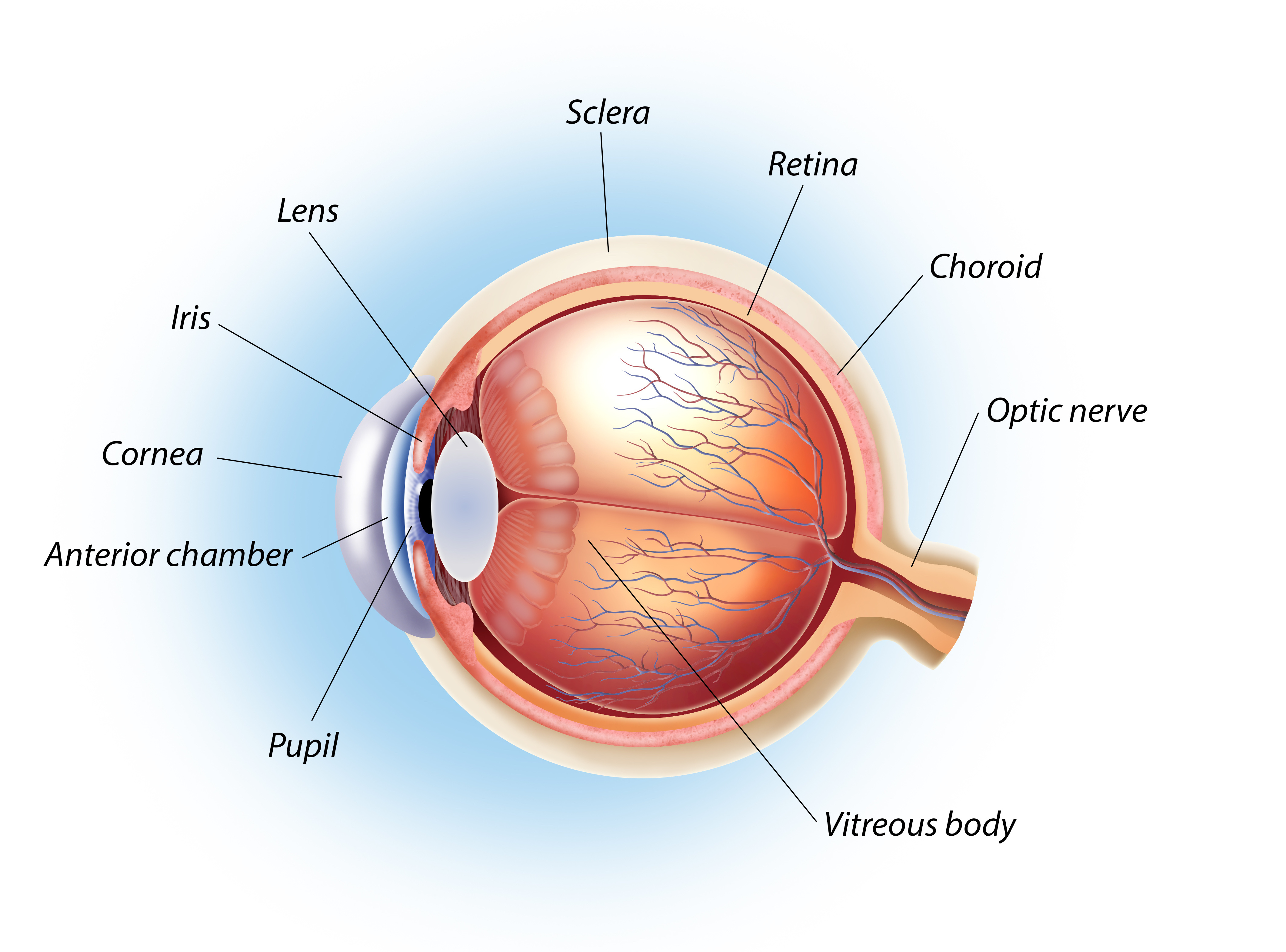
Corneal ectasia refers to a group of conditions that cause the progressive thinning of the cornea (clear front layer of the eye). This thinning causes the corneal tissue to weaken and bulge outward.
Ectasia can occur on its own, or it can result from certain surgeries, such as corneal refractive surgery. The main symptom is blurry or distorted vision that worsens over time.
What Are the Types of Corneal Ectasia?
The types of corneal ectatic disorders are:
- Keratoconus. The most common type, this disease causes gradual thinning of the central cornea. The weak cornea causes the eye to bulge in the shape of a cone.
- Posterior keratoconus. A rare but non-progressive condition. It causes thinning at the inner surface (posterior) of the cornea. Unlike keratoconus, it does not lead to a cone-shaped bulging of the eye.
- Keratoglobus. A rare and degenerative eye disorder with general thinning of the cornea. It causes round-shaped (globular) bulging of the eyes.
- Pellucid marginal degeneration (PMD). A degenerative form of corneal ectasia. It causes thinning on the lower portion and sides of the cornea.
- Terrien marginal degeneration (TMD). A slowly progressive eye disease that causes peripheral thinning of the cornea.
- Post keratorefractive ectasia. A post-surgical corneal ectasia that occurs as a complication of LASIK or PRK.
- Wound ectasia after penetrating keratoplasty (PK). A corneal ectatic disorder that develops as a complication of a corneal transplant.
- Post-LASIK ectasia. Though rare, corneal ectasia is a devastating complication of LASIK surgery.
Is Corneal Ectasia a Risk After LASIK?
Yes. Post-LASIK ectasia is a rare but serious complication that affects 0.02% to 0.6% of people who undergo LASIK.1 It can cause progressive myopia and astigmatism, leading to worsening eyesight.
LASIK surgery uses a special laser to cut and shape the cornea. If too much corneal tissue is removed or damaged, it can cause ectasia. People with pre-existing corneal problems may also develop post-surgical corneal ectasia.2
Before the procedure, your doctor will assess you to see if you are a suitable candidate. The ophthalmologist will also discuss the benefits and risks of LASIK surgery.
What Is the Difference Between Ectasia and Keratoconus?
Corneal ectasia is a group of eye conditions that involve corneal thinning. Keratoconus is the most common type of corneal ectasia. In people with keratoconus, the thin corneal tissue bulges outward like a cone.
What Are the Symptoms of Corneal Ectasia?
The symptoms of corneal ectasia can vary for each person. It usually depends on the damage sustained by the cornea.
Corneal ectasia typically causes gradually worsening vision. Unless treated, it can lead to vision loss.
Common corneal ectasia symptoms include:
- Astigmatism or blurred vision at all distances
- Myopia or nearsightedness (blurring of distant objects)
- Changes in the shape of the cornea (coned or globular)
- Seeing glare, halos, and starbursts around lights
- Diplopia or double vision and ghosting
- Watery eyes
- Light sensitivity
- Failed attempts to correct vision problems with glasses or contacts
Who Gets Corneal Ectasia?
Corneal ectasia affects people of all ages, sexes, and ethnicities. The typical age of onset varies depending on the type:
- Keratoglobus. Occurs in children and teens
- Keratoconus. Occurs in teens and young adults
- Pellucid marginal degeneration (PMD). Usually begins in the 20s, 30s, or 40s
- Post-LASIK ectasia. Can occur months or years after LASIK surgery
What Causes Corneal Ectasia?
Corneal ectatic diseases can occur naturally. Sometimes, corneal ectasia is a complication of eye surgery, such as laser vision correction.
Most corneal ectasias are present in families. This suggests it’s a hereditary condition.3,4
Corneal trauma is another possible cause. External factors such as eye surgery, contact lenses, and frequent and aggressive eye rubbing have been associated with ectasia.3,4,5
Risk Factors
Factors that increase your risk for corneal ectasia are:
- Age and gender. TMD is common in middle-aged men5
- Congenital diseases. Includes Down's syndrome, albinism, and retinitis pigmentosa
- Connective tissue disorders. Includes Marfan, Rubinstein-Taybi Syndrome, and Ehlers-Danlos Syndrome
- Allergic conditions. Such as asthma, allergies, eczema, and hay fever
- Inflammatory diseases. Like idiopathic orbital inflammation and thyroid eye disease
- Medications. Systemic or topical corticosteroid use6
How Is Corneal Ectasia Diagnosed?
An eye specialist can diagnose corneal ectasia through a comprehensive eye exam and clinical tests. First, they will review your medical history and ask about your family history of eye diseases.
Tests that can help diagnose corneal ectasia include:
- Slit-lamp exam. Your eye specialist will use a special microscope with a bright light to examine all parts of your eye.
- Keratometry. This test measures the radius of the corneal curvature to check for an irregular astigmatism or corneal steepening.
- Corneal topography. This imaging test maps the surface of the cornea to check for distortions in its curvature.
- Corneal tomography. This non-invasive test takes cross-section images of the front part of the eye to easily check the size, thickness, and shape of different corneal structures.
- Corneal pachymetry. This simple test measures corneal thickness at different points.
How Is Corneal Ectasia Treated?
Treatment options for corneal ectasia include:
Eyeglasses
Glasses can correct mild cases of non-progressive corneal ectasia. Studies show that eyeglasses can improve your vision by up to 20/20 or 20/40.6
Contact Lenses
Your ophthalmologist may prescribe different lenses, depending on your diagnosis:
- Soft contact lenses. They can improve the vision of people with mild keratoconus.
- Rigid gas-permeable lenses (RGP). Often prescribed as an alternative to eyeglasses that can no longer get your vision up to 20/30.
- Hybrid lenses. They have an RGP center and a soft skirt. Doctors recommend it as an alternative for people with RGP intolerance.
- Piggyback contact lenses. This treatment involves wearing RGP contact lenses on top of soft contacts. It is more comfortable and can prevent corneal damage.
- Scleral lenses. Can be custom-made to fit your eyes. A scleral lens improves visual acuity by clearing the cornea and improving the focus and stability of light.
Corneal Cross-Linking (CXL)
Corneal collagen cross-linking is a minimally invasive surgical procedure. It slows the thinning of the cornea in progressive forms of ectasia.
CXL strengthens and stabilizes the cornea, which helps delay corneal thinning. It can treat mild to moderate cases of keratoconus and post-surgical corneal ectasia.6
Intracorneal Ring Segment Implantation (ICRS)
Also known as intrastromal corneal ring segments or corneal implants, these are small, clear, and crescent-shaped implants. It is a minimally invasive procedure that involves the insertion of intracorneal ring segments into the cornea.
An intracorneal ring can flatten abnormally steep cornea. It treats post-LASIK ectasia and keratoconus.9 Some eye surgeons combine IRCS with CXL to improve outcomes.
Corneal Transplant
Corneal transplantation or keratoplasty is an invasive eye surgery. It is the mainstay treatment for severe corneal ectasia. Keratoplasty is an option if optical devices like eyeglasses and contact lenses no longer correct your ectasia.
There are two types of corneal transplants:
- Penetrating keratoplasty. The entire cornea is replaced.
- Lamellar keratoplasty. Replaces the front and middle layers of the cornea.
Most surgeons prefer lamellar keratoplasty if the back of the cornea is healthy.
How to Prevent Corneal Ectasia
Most forms of corneal ectasia aren’t preventable. However, an early diagnosis can help reduce your risk for factors that might speed up disease progression.
Here’s how to ensure an early diagnosis:
- Get regular eye exams
- Before undergoing vision correction surgery, talk to your doctor about your risk assessment for corneal ectasia
- Find out if any family members have a history of corneal ectasia
Summary
Corneal ectasia is a group of eye disorders that cause the cornea to become progressively thinner. This causes the cornea to weaken and bulge. The most common symptom of corneal ectasia is blurred vision that worsens gradually.
Most types of corneal ectasia occur naturally and aren’t preventable. Ectasia can be a rare but severe complication of certain eye surgeries, such as LASIK. Talk to your doctor about your risk factors for corneal ectasia before undergoing LASIK or any laser refractive surgery.
In this article
15 sources cited
Updated on February 20, 2024
Updated on February 20, 2024
About Our Contributors
Dr. Melody Huang is an optometrist and freelance health writer with a passion for educating people about eye health. With her unique blend of clinical expertise and writing skills, Dr. Huang seeks to guide individuals towards healthier and happier lives. Her interests extend to Eastern medicine and integrative healthcare approaches. Outside of work, she enjoys exploring new skincare products, experimenting with food recipes, and spending time with her adopted cats.
