Updated on October 31, 2024
What is Periorbital Cellulitis?


Vision Center is funded by our readers. We may earn commissions if you purchase something via one of our links.
Periorbital cellulitis is a common eye infection that can cause significant discomfort and potential complications if left untreated.
In this article, we'll discuss the causes, symptoms, diagnosis, and treatment of periorbital cellulitis, providing valuable information for early detection and effective management of this condition.
What Is Periorbital Cellulitis?
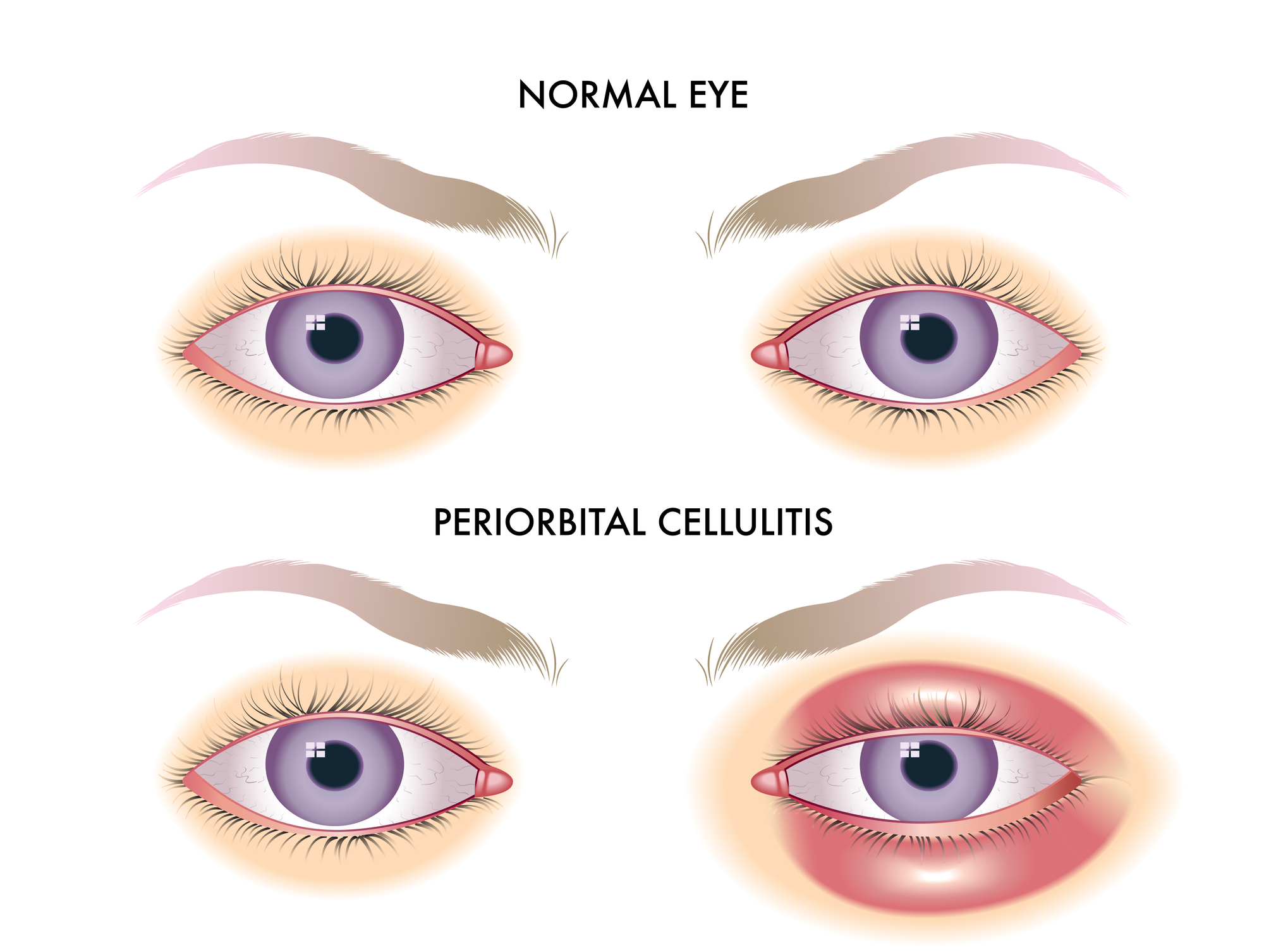
Periorbital cellulitis is an eye infection that affects the eyelid or surrounding areas. It’s also referred to as preseptal cellulitis.
It’s mainly characterized by eyelid swelling and manifests after an eye injury. It can also develop if the bacteria inside a stye spreads.
This infection resembles a rare but more severe condition called orbital cellulitis. This one affects the eyeball and the surrounding tissues.
Recent studies have shown that periorbital and orbital cellulitis can occur at any age. However, it is more common among children (pediatric periorbital cellulitis).
What Causes Periorbital Cellulitis
For the infection to develop, infectious agents must contact the eye tissues. These include:
- Bacteria
- Viruses
- Parasitic worms
- Fungi (rare cases)
The majority of periorbital cellulitis cases are due to bacterial infections. A bacterial infection may spread from a sinus infection (sinusitis) or another eye area.
It can also happen due to minor trauma to the eyelids, such as a bug bite or an accidental scratch. However, it might also occur due to upper respiratory infection or dental abscess.
What Bacteria Cause Periorbital Cellulitis?
The most common bacteria that can cause periorbital cellulitis are methicillin-resistant Staphylococcus aureus (MRSA), streptococcus pneumoniae, streptococcus pyogenes, and haemophilus influenzae.
Less common causative bacteria include:
- Acinetobacter
- Bacillus
- Mycobacterium
- Pseudomonas
- Neisseria
- Nocardia
- Proteus
- Pasteurella
In rare cases, fungi such as Mucorales and Aspergillus can cause periorbital cellulitis.
What are the Symptoms of Periorbital Cellulitis?
Periorbital cellulitis typically affects one side of the face. Common symptoms include:
- Eyelid swelling
- Red-eye
- Eye pain
- Tenderness to touch
- Difficulty opening the affected eye
- Discoloration of the eyelid
- Fever (less common)
- Teary eyes
- Eye discharge (less common)
- Decreased vision (less common)
According to the British Association of Dermatologists, infected white skin may appear pink or red. On the other hand, black and brown skin may appear purple.
When Should You See A Doctor for Periorbital Cellulitis?
Periorbital cellulitis can be a dangerous infection. It can spread to other areas and cause complications. With proper treatment, you can stop the spread of the infection.
Below are signs that you need to contact a doctor:
- If your eye swells or becomes red
- If you notice an injury or tenderness of the skin around the eye
- If a fever develops
- If your eye looks like it’s bulging outwards (proptosis)
This condition may not be accompanied by pain or fever. However, if you or a loved one is experiencing fever and swelling and it’s difficult to open or move the affected eye, seek professional advice from your healthcare professional.
Complications
Unlike orbital infections, periorbital cellulitis does not affect the eyeball. However, if left untreated, it may lead to serious complications like:
- Orbital cellulitis. It’s more severe and accompanied by bulging of the eye (proptosis) eyes and vision impairment.
- Orbital abscess. This is the development of pus within the orbital tissue.
- Cavernous sinus thrombosis. This is a blood clot that forms in the sinuses and ends up affecting the second eye. It can progress to intracranial infection.
- Vision problems or blindness. As the infection spreads, it impairs essential parts that enable your eyes to see.
Additionally, orbital cellulitis may lead to life-threatening conditions, like sepsis (extreme response to an infection) and meningitis.
Treatment Options for Periorbital Cellulitis
The treatment choices will be determined by the person’s age and the stage of the infection. Previously, periorbital cellulitis was treated using amoxicillin-clavulanic acid, cefpodoxime, or cefdinir.
However, the rise of methicillin-resistant Staphylococcus aureus (MRSA) has changed how this infection is treated. The currently recommended treatment options are:
- Clindamycin
- Trimethoprim-sulfamethoxazole (TMP-SMX)
- Doxycycline
Doctors will give oral antibiotics for infections in patients over one year old. However, infants less than a year old suffering from a severe infection will be hospitalized. Those who are hospitalized are given intravenous (IV) antibiotics.
The antibiotics should start working within 24 to 48 hours. However, you may need a follow-up visit to ensure the infection is completely gone.
How Periorbital Cellulitis is Diagnosed
If your doctor suspects periorbital cellulitis, they’ll begin with a physical examination of your eyes for signs of injury. Your doctor may examine your eye movements and response to light.
They’ll use tools such as X-rays and CT scans to get a clear picture of the infected area. But, if your doctor suspects that an underlying problem is causing the infection, they’ll do further investigation.
In this case, they may take a fluid sample, such as blood cultures, from the affected eye or other areas to determine the type of bacteria causing the problem. Once your doctor identifies the bacteria causing your eye infection, they will then proceed to administer treatment.
In this article
9 sources cited
Updated on October 31, 2024
Updated on October 31, 2024
About Our Contributors
Vincent Ayaga is a medical researcher and seasoned content writer with a bachelor's degree in Medical Microbiology. Specializing in disease investigation, prevention, and control, Vincent is dedicated to raising awareness about visual problems and the latest evidence-based solutions in ophthalmology. He strongly believes in the transformative power of ophthalmic education through research to inform and educate those seeking knowledge in eye health.
Dr. Melody Huang is an optometrist and freelance health writer with a passion for educating people about eye health. With her unique blend of clinical expertise and writing skills, Dr. Huang seeks to guide individuals towards healthier and happier lives. Her interests extend to Eastern medicine and integrative healthcare approaches. Outside of work, she enjoys exploring new skincare products, experimenting with food recipes, and spending time with her adopted cats.

