Updated on October 9, 2024
Ocular Rosacea - Symptoms, Causes, Diagnosis & Treatment


Vision Center is funded by our readers. We may earn commissions if you purchase something via one of our links.
What is Ocular Rosacea?
Ocular rosacea, which can cause meibomian gland dysfunction (MGD), is a prevalent inflammatory condition affecting the eye surface. It's often associated with rosacea, a chronic skin condition characterized by redness and irritation.1
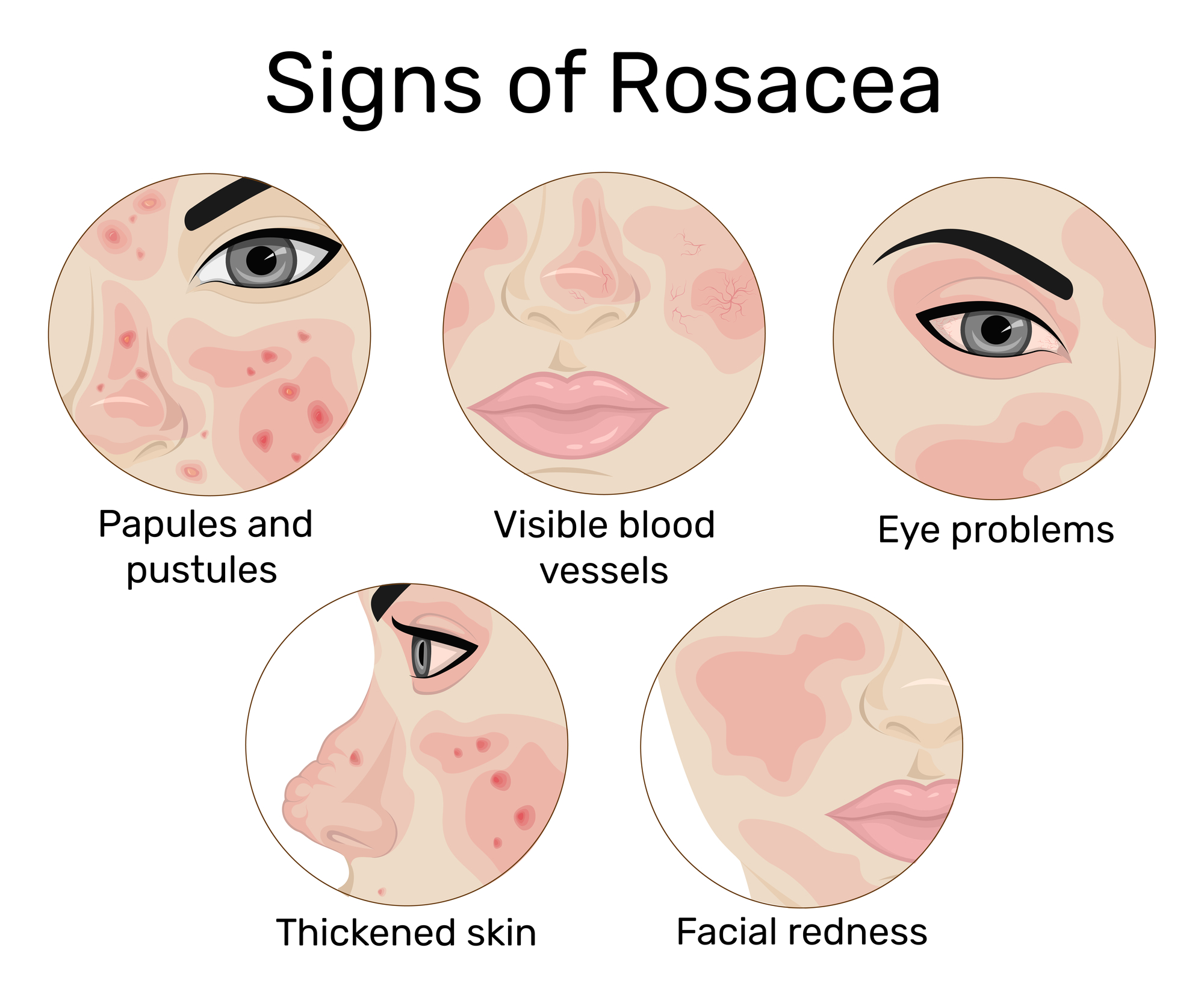
Symptoms of ocular rosacea include:
- Redness
- Watering
- Burning sensations
- Dry, sensitive feeling in the eyes
While ocular rosacea commonly occurs in individuals with rosacea, it can also manifest independently. In some cases, eye symptoms may precede skin symptoms, occurring approximately 15% of the time.
Approximately 5.5% of the adult population has rosacea.2 It’s most common in females. However, ocular rosacea is less common, affecting less than 1% of people.3
Anyone can develop ocular rosacea, but it's most common after age 30 and typically seen between ages 40 and 59.
No known cure for ocular rosacea exists, but treatment options exist. It’s crucial to seek medical attention for ocular rosacea symptoms as it can lead to permanent vision loss.4
What are the Symptoms of Ocular Rosacea?
Some ocular rosacea symptoms include:3
- Red, bloodshot eyes
- Watering eyes
- Dry, burning, or itchy eyes
- Vision sensitivity
- Blurred vision
- Dilated small blood vessels on the white of the eye
- Swollen eyelids
- Feeling of grittiness
Ocular rosacea may be associated with other eye conditions:
- Chalazion or stye
- Eye infections such as conjunctivitis (pink eye) or blepharitis
- Corneal ulceration
When to See a Doctor
If you experience eye problems or develop symptoms of ocular rosacea, you should see your primary care provider. They can prescribe medications or refer the person to an ophthalmologist.
An ophthalmologist or an optometrist with specialized training in ocular surface diseases and inflammation can be considered an ocular rosacea specialist.
Early diagnosis and treatment are essential to prevent severe ocular rosacea and further eye damage.
Diagnosis
Diagnosing ocular rosacea can be challenging as there are no specific tests. Therefore, doctors diagnose the condition based on medical history, symptoms, and a clinical exam. They may take a skin scraping or eyelash sample to confirm the presence of eyelash mites.
Doctors may suspect ocular rosacea if someone has skin rosacea and eye symptoms. However, it can be challenging to diagnose without skin problems. Many of the symptoms of ocular rosacea are nonspecific.
Potential Complications
A person can develop an inflamed cornea (keratitis) without proper ocular rosacea treatment. Although rare, ocular rosacea can cause this complication.
With each episode of keratitis, the cornea becomes thinner and more opaque as blood vessels form. Sometimes this can lead to deep ulcers and perforation. It could also lead to vision loss.
Although rare, other complications of ocular rosacea include:
- Inflammation of the iris (iritis)
- Inflammation of the clear tissue lining the inner eyelids and sclera (episcleritis)
- Inflammation of the white of the eye (scleritis)
Treatment for Ocular Rosacea
Treatment for ocular rosacea may depend on the severity of someone's symptoms. Doctors may recommend eye drops, systemic medications, surgery, and home remedies.
Professional Treatment Options
Doctors may prescribe topical antibiotics or antibiotic eye drops. These may include:
- Azithromycin
- Bacitracin
- Erythromycin
- Metronidazole
They may also recommend topical medications such as non-steroidal anti-inflammatory agents and steroid eye drops to relieve inflammation. Topical steroids are only suitable for short-term use. In the long-term, they can lead to glaucoma and cataracts. If symptoms don't improve with topical steroids, topical cyclosporine is an alternative.
Systemic medications
Oral antibiotics may help:
- Reduce the number of bacteria
- Improve the tear film
- Reduce inflammation
- Regulate secretions from the eyes' oil glands (meibomian glands)
Doctors may recommend tetracyclines such as doxycycline or macrolides such as erythromycin. People typically take these antibiotics for up to three months and then taper the dose over two months.
Oral antibiotics may also help if the person has a stye that doesn't clear with topical antibiotics.
Another treatment option to consider is oral retinoids, such as isotretinoin. However, isotretinoin may exacerbate ocular rosacea due to its potential side effects, which include dry eyes and increased susceptibility to infections.
Surgery
If someone has corneal complications such as scarring or perforation, surgery may help. A keratoplasty or corneal transplant replaces part or all of the cornea with tissue from a donor.
Doctors may also remove styes with surgery if they don't improve with warm compresses and antibiotics.
Home Remedies
Some home remedies may help relieve the symptoms of ocular rosacea, including:
- Keeping the eyelids clean. Use a damp cotton bud and diluted baby shampoo or bicarbonate of soda to clean the eyelids and eyelashes gently. This helps remove skin scales and bacteria.
- Applying a warm compress. Sitting with a warm, damp washcloth or cotton ball on the closed eyelids for five minutes can help with styes and cysts.
- Using artificial tears. Pharmacies sell artificial tears that can lubricate the eyes and relieve dryness.
- Avoiding wearing contact lenses. People who wear contact lenses should swap to eyeglasses to prevent irritation of inflamed eyes.
- Taking omega-3 fatty acid. Research suggests these supplements may help dry eyes.6
Outlook
Ocular rosacea is a condition with no cure. Although the symptoms can be uncomfortable, medications and home remedies can help control them.
There are some serious complications associated with ocular rosacea. Therefore, anyone experiencing eye or visual symptoms should speak to their doctor or ophthalmologist.
Risk Factors of Ocular Rosacea
Having skin rosacea is one of the main risk factors for ocular rosacea. However, it can occur without skin involvement.
The risk factors for skin rosacea include being female and Caucasian. Researchers believe there is a genetic link.
In contrast, ocular rosacea affects men and women equally. It's also more common in fair-skinned people of Celtic and Northern European origin.
What Causes (or Triggers) Ocular Rosacea?
The exact cause of ocular or skin rosacea is unknown. However, in almost 6 in 10 cases, ocular rosacea is associated with skin rosacea.2
Other potential causes include:
Mites and Microorganisms
Demodex mites frequently inhabit eyelash follicles. These tiny mites may trigger inflammation or block the eyelid glands.5
Inflammatory Markers
An inflammatory protein called interleukin 1-alpha (IL-1α) is increased in tears and can inflame and damage eye tissue.
Bacteria
Ocular rosacea may improve with antibiotics indicating that bacteria play a role. Doctors also believe Helicobacter pylori bacteria, which also causes gastrointestinal infections, may be involved in ocular rosacea.
Food and Environmental Factors
Certain foods and environmental factors can also trigger a rosacea flare-up and worsen symptoms. These include:
- Exposure to heat, sun, wind, or cold
- Taking saunas or hot baths
- Strenuous activities such as running
- Drinking alcohol, hot coffee, or tea
- Eating hot or spicy foods or dairy products
- Emotions such as stress and feeling sad
- Some medications, such as cortisone cream
Additionally, some systemic disorders are associated with rosacea. These include high blood pressure and abnormal blood fat levels.
Can You Prevent Ocular Rosacea?
No, you can't prevent ocular rosacea, but you may be able to prevent flare-ups.
Some people find that certain beverages, alcohol, sunlight, or other triggers can aggravate symptoms. Therefore, keeping a symptom diary to identify and avoid potential triggers is a good idea.
Additionally, doctors may recommend that people with skin rosacea undergo periodic eye exams to assess their visual health. By doing so, any problems can be caught early on and treated.
Summary
Ocular rosacea is an inflammatory eye condition. It causes redness, swollen eyelids, and blurred vision, among other symptoms. The condition often develops in people with skin rosacea, but not always.
The cause of ocular rosacea is unknown, but genetics, bacteria, and other health conditions may contribute.
There is no cure for ocular rosacea, but various treatments can help ease symptoms. These include good eyelid hygiene, eye drops, and oral medications.
If you're experiencing symptoms of ocular rosacea, speak with a doctor. Prompt and proper treatment reduces the risk of complications.
In this article
6 sources cited
Updated on October 9, 2024
Updated on October 9, 2024
About Our Contributors
Zia, with a Master's in Public Health from the University of Manchester and over a decade of experience as a health and wellness copywriter and digital health journalist, specializes in a range of topics from public health to ophthalmology. Her mission is to empower and educate about visual health through engaging, evidence-based writing. In her leisure time, Zia loves traveling and spending playful moments with her dogs.
Dr. Melody Huang is an optometrist and freelance health writer with a passion for educating people about eye health. With her unique blend of clinical expertise and writing skills, Dr. Huang seeks to guide individuals towards healthier and happier lives. Her interests extend to Eastern medicine and integrative healthcare approaches. Outside of work, she enjoys exploring new skincare products, experimenting with food recipes, and spending time with her adopted cats.

