Updated on October 9, 2024
What is Age-Related Macular Degeneration? Causes, Prevention, & Treatment


Vision Center is funded by our readers. We may earn commissions if you purchase something via one of our links.
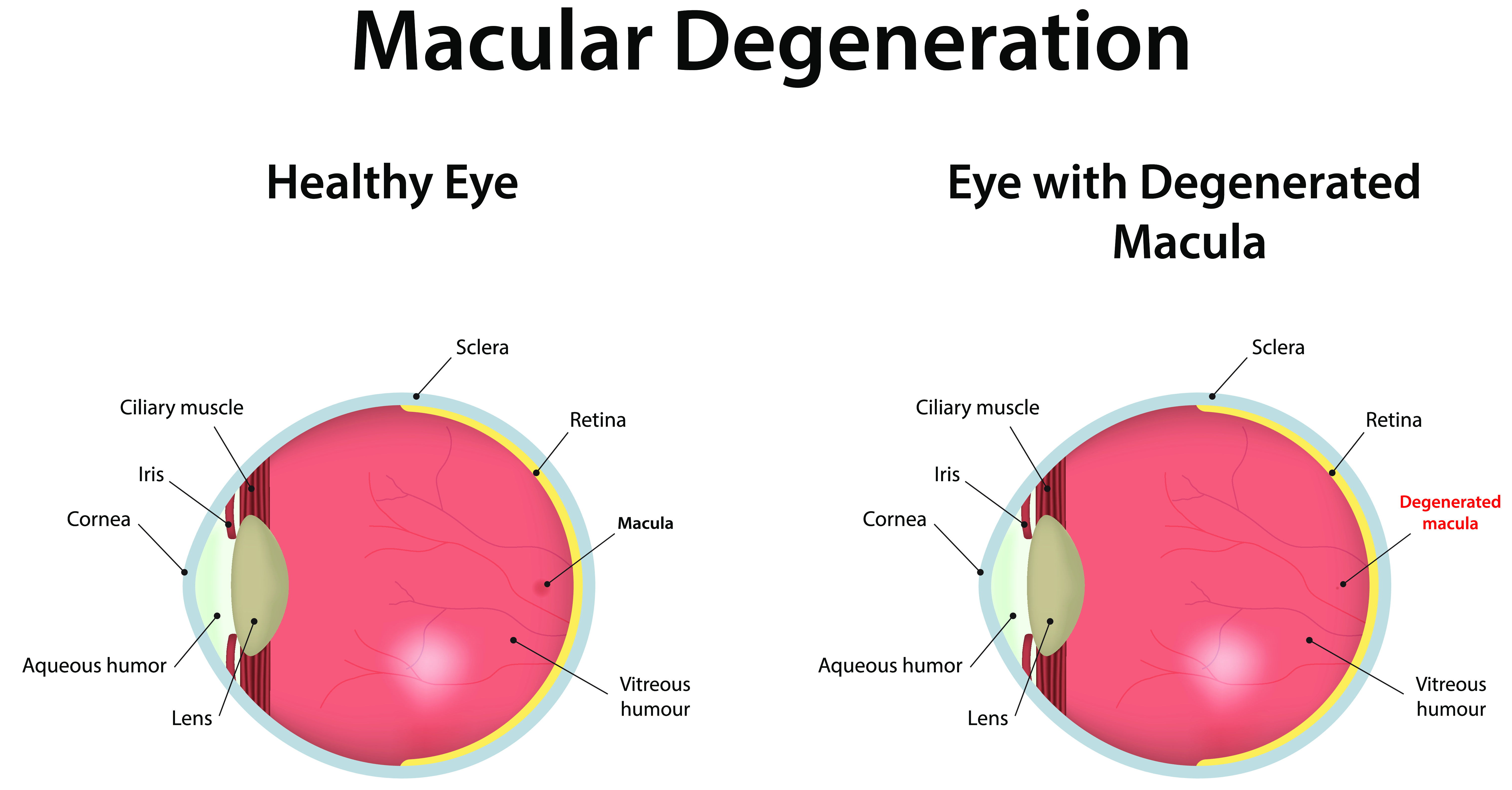
Macular degeneration or age-related macular degeneration (AMD) is an ocular disease that affects central vision. It occurs when the central portion of your retina, the macula, wears down.
The macula is responsible for central vision and helps send information from the optic nerve to the brain. It controls your ability to:
- Read
- Drive
- Recognize faces and colors
- See objects in refined detail
When the cells of your macula deteriorate, you begin to lose central vision but retain peripheral vision. Macular degeneration can affect one or both eyes. However, it's unlikely to cause total blindness.
Symptoms of Age-Related Macular Degeneration
Age-related macular degeneration worsens over time.2 Because the early stages of macular degeneration may have no symptoms, it can be difficult to notice until it progresses.
However, as the disease progresses, you may notice a change in visual acuity. These changes will be more significant if the condition affects both eyes.

Signs and symptoms of AMD include:
- Need for brighter lighting to read
- Blurred vision
- Decreased vision
- Straight lines appearing bent or wavy
- Dark or blurry areas in the center of your vision
- Difficulty recognizing faces
- Reduced brightness or intensity of colors
Symptoms of Dry Macular Degeneration
Dry macular degeneration progresses more slowly and is less likely to result in significant loss of vision or other problems. Changes in blood vessels are also less severe in dry macular degeneration.
Symptoms include:
- Retinal damage
- Blurry vision
- Difficulty recognizing faces
- Straight lines that now appear wavy or bent
- Blindspot near the central vision
- Change in color perception (rare)
- Light sensitivity
- Loss of central vision
- Vision loss
Symptoms of Wet Macular Degeneration
Wet macular degeneration symptoms are similar to dry macular degeneration symptoms. People with wet AMD lose their central vision more quickly than those with dry AMD.
Other symptoms include:
- A dark spot in the central vision due to leaking vessels
- Hazy vision
- Rapidly worsening symptoms
- Vision loss
Types of Age-Related Macular Degeneration
There are two types of macular degeneration: dry (non-exudative) and wet (exudative). There's also a rare form of macular degeneration that develops in children and teenagers called Stargardt disease.
Here are their differences:
Dry Age-Related Macular Degeneration
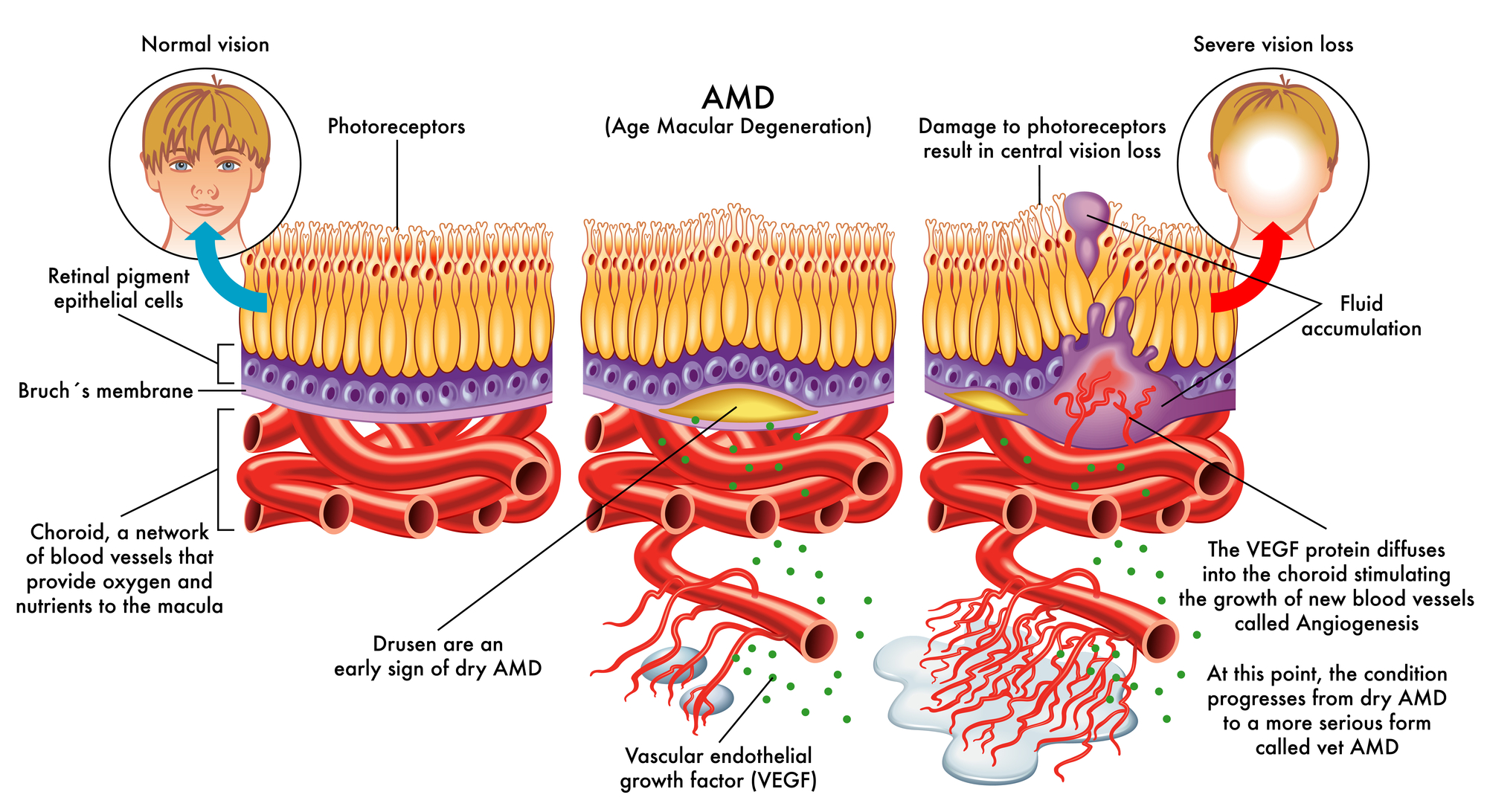
The dry form of macular degeneration is the most common type. About 80 to 90 percent of all AMD cases are dry.3
Dry macular degeneration is characterized by the gradual thinning of the macula and the formation of tiny yellow protein clumps (drusen).10 The presence of large drusen signifies more advanced macular degeneration.
As the eye disease progresses, the light-sensitive cells in your macula wear away and eventually die. This can cause blind spots in your central vision.
Wet Age-Related Macular Degeneration
Wet macular degeneration occurs when abnormal and new blood vessels form beneath the retina.9 As a result, blood or other fluids may leak from these vessels and cause macular damage.
In some cases, advanced dry AMD may become wet AMD. Eventually, these abnormal blood vessels and their fluids will form scars. This results in permanent central vision loss. Wet AMD often results in more severe vision loss than dry cases.
What is Stargardt Disease?
In rare cases, AMD will develop in children or teenagers. This is known as Stargardt disease. While Stargardt disease is similar to AMD, it is thought to be caused entirely by genetics.
What Causes Macular Degeneration?
Generally, macular degeneration affects older people. However, the exact cause of AMD is still unknown.
Researchers believe there are genetic components and environmental factors that may affect your susceptibility to AMD. This means you're likely to develop AMD if your family has a history of the condition.
Other age-related macular degeneration risk factors include:10
- Gender: Women are at a higher risk of developing AMD than men
- Race: People of European and North American ancestry are more likely to develop macular degeneration than people of Hispanic, Asian, or African ancestry
- Smoking: Smoking or being exposed to second-hand smoke increases your chances of developing AMD
- Unhealthy Diet: Research suggests obesity, high cholesterol, and unhealthy diets may increase the severity of AMD
- Cardiovascular disease: Conditions affecting the heart or blood vessels (e.g., high blood pressure) are more likely to cause a wet form of macular degeneration
How Common Is Age-Related Macular Degeneration (AMD)?
Age-related macular degeneration is the most common cause of vision loss in adults older than 60.2,4,7 AMD is common among people over 50.1
AMD affects more than 11 million people in the U.S. and over 190 million worldwide.7 Men and women are equally susceptible to developing it, and increasing age is the greatest risk factor.
3 Stages of Macular Degeneration
There are three stages of macular degeneration. People with early and intermediate AMD usually don’t experience symptoms. They typically learn they have AMD during a routine eye exam.
1. Early AMD
In the early stage of macular generation, the disease affects your macula but not your vision. Most people don't experience vision loss in the early stages.
However, objects may appear blurry. You may also see straight or wavy lines. An eye doctor can diagnose early AMD during an eye exam by spotting medium-sized drusen (yellow deposits) in the macula.
2. Intermediate AMD
During the intermediate stage of macular degeneration, you may experience reduced central vision. It can be difficult to see faces from far away, and colors may appear duller.
However, not everyone will experience vision problems yet. Optometrists will perform an eye examination for larger drusen or pigmentation changes in the retina.
3. Late AMD
During late or advanced-stage AMD, vision loss has become noticeable. There may be permanent thinning or scarring of cells.
You aren't able to drive, read, or recognize faces anymore. You may also experience severe visual hallucinations during this stage.
When to See a Medical Professional
Schedule an eye exam immediately if you experience any of these symptoms. Undergo an annual eye examination, especially after age 50, to maintain proper eye health.
Because AMD isn't detectable in the early stages, it's important to have regular eye exams. This can help detect early symptoms, especially if you're at risk for AMD. If you have age-related macular degeneration, observe your eyes daily and tell your doctor if you notice any vision changes.
How is AMD Diagnosed?
AMD is diagnosed during a complete eye examination. If you are at risk for AMD, they may perform one or more tests to check for signs of macular degeneration:
Amsler Grid

Your ophthalmologist may also ask you to look at an Amsler grid.7 This is a checkerboard-like pattern of straight lines.
This will test for deficiencies in your central vision. If some of the straight lines in the Amsler grid appear wavy, broken, or faded, this may be a sign of macular degeneration.
Retinal Examination
Age-related macular degeneration is detectable during a routine eye exam. Your eye doctor may dilate your pupils by administering eye drops.
They will then use a special instrument to examine the back of your eye. This can help them look for drusen under the retina.
Fluorescein Angiography
This involves your doctor injecting a colored dye into your arm. The dye travels to the blood vessels in your eye.
A camera will take several pictures as the dye highlights the blood vessels. The images will reveal if you have abnormal blood vessels or changes in your retina.
Optical Coherence Tomography (OCT)
Your ophthalmologist might also recommend optical coherence tomography (OCT). During an OCT exam, your eye doctor will use a particular machine to capture ultrasound images of the inside of your eye.
This painless, non-invasive imaging procedure will take detailed cross-sectional images of your retina, including the macula. It will identify areas of retinal thinning, thickening, or swelling.
Macular Degeneration Treatment Options
There is no known cure for age-related macular degeneration. However, there are many treatment options, depending on the type and severity of your condition.
Early treatment can help slow the progression of AMD and reduce the severity of your symptoms. However, symptoms often return even if treatment is successful.
These are the possible treatment options for macular degeneration:
1. Nutritional Therapy
Clinical trials show that taking nutritional supplements helps people with intermediate or late AMD.1 The original Age-Related Eye Disease Studies (AREDS) formula for nutritional supplementation contains a combination of vitamins and minerals.
These include:
| Nutrient | Amount |
| Vitamin C | 400 mg |
| Vitamin E | 400 IU |
| Beta-carotene | 15 mg |
| Copper (cupric oxide) | 2 mg |
| Zinc | 80 mg |
The AREDS2 formula was modified to remove beta-carotene, which increased smokers’ chances of lung cancer:
| Nutrient | Amount |
| Vitamin C | 400 mg |
| Vitamin E | 400 IU |
| Copper (cupric oxide) | 2 mg |
| Lutein | 10 mg |
| Zeaxanthin | 2 mg |
| Zinc | 80 mg |
The vitamins C and E, beta-carotene, zinc, copper, lutein, zeaxanthin, and omega-3 fatty acids have all been linked to reducing the risk of vision loss. Your doctor may prescribe nutritional supplements containing antioxidant vitamins. These can help combat the progression of AMD.
2. Anti-VEGF Injections
Anti-VEGF (vascular endothelial growth factor) drugs are currently the most common and effective treatment for AMD. This drug is injected into the eye and stimulates the growth of new blood vessels.
This procedure takes approximately 15 minutes. It has shown great potential in slowing down and even preventing macular degeneration progression.
Examples include:
- Aflibercept (Eylea)
- Bevacizumab (Avastin)
- Ranibizumab (Lucentis)
3. Photodynamic Laser Therapy
Laser therapy or laser surgery can reduce the symptoms of macular degeneration. PDT combines injections and laser treatment to reduce macular degeneration symptoms.
The injection contains a photosensitizing drug, which is activated by the laser. It helps destroy abnormal blood vessels and slow down vision loss.
However, laser therapy has not proven successful in the long-term. The procedure will likely need to be repeated.
4. Low-Vision Aids
Low-vision devices improve vision for people who suffer from poor vision. They can be optical, non-optical, or electronic. There are several instruments and techniques available, such as magnifiers and low-vision optical lenses.
How to Prevent Macular Degeneration
Studies show that non-smokers and those who maintain a proper diet have a lower risk of developing AMD.13 You can also prevent macular degeneration by:
- Managing your other medical conditions, if applicable
- Taking supplements rich in vitamins, Omega-3, zinc, copper, lutein, and zeaxanthin
- Quitting smoking
- Exercising regularly
- Maintaining healthy cholesterol levels and blood pressure
- Avoid processed foods. Instead, opt for a diet rich in antioxidants and healthy fats, such as the Mediterranean diet
Age-Related Macular Degeneration Research and Outlook
If you’re diagnosed with macular degeneration, don’t lose all hope. The National Eye Institute has been researching age-related macular degeneration (AMD).
For instance, the NEI hopes they can use pharmacologic, stem cell, and gene therapy-based strategies for macular degeneration treatment in the future. They hope their research will lead to a greater understanding of how the disease works and how it can be treated.
Summary
Age-related macular degeneration (AMD) is an eye disease that affects central vision (the ability to see finer details). It damages the macula and the retina, leading to eventual vision loss.
There are two types of macular AMD: dry and wet. Both conditions result in retinal damage, blurry vision, blind spot, light sensitivity, and central vision loss.
While no cure is available for macular degeneration, there are many ways to manage its symptoms. Consult an eye doctor to determine the best treatment for your situation, especially if you're at risk of AMD.
In this article
7 sources cited
Updated on October 9, 2024
Updated on October 9, 2024
About Our Contributors
Michael, a lead content writer for Vision Center, brings eight years of experience in medical copywriting and advanced research methodologies. With a B.A. in English and Linguistics from the University at Buffalo, he specializes in creating detailed, evidence-based content, particularly in the field of eye health, to educate readers and guide them toward appropriate treatments.
Dr. Melody Huang is an optometrist and freelance health writer with a passion for educating people about eye health. With her unique blend of clinical expertise and writing skills, Dr. Huang seeks to guide individuals towards healthier and happier lives. Her interests extend to Eastern medicine and integrative healthcare approaches. Outside of work, she enjoys exploring new skincare products, experimenting with food recipes, and spending time with her adopted cats.

