Updated on March 25, 2025
How Do Chronic Conditions Affect Eye Health? (2025)


Vision Center is funded by our readers. We may earn commissions if you purchase something via one of our links.
Chronic diseases have far-reaching effects on overall well-being, and their impact on eye health is significant and multifaceted. In this article, we explore how conditions such as diabetes, hypertension, and chronic kidney disease have influenced vision outcomes in the United States over the past decade.
Over the past ten years, researchers and public health experts have documented a clear connection between chronic illnesses and the onset or worsening of eye disorders. This analysis brings together data on disease correlations, treatment and prevention effectiveness, healthcare costs, and long-term patient outcomes to offer a comprehensive picture of how systemic conditions are linked with ocular health challenges.
Key Statistics
- 29% of U.S. adults over 40 with diabetes are affected by diabetic retinopathy, the leading cause of blindness in working-age adults.
- Effective blood sugar control in diabetic patients can reduce the risk of developing diabetic eye disease by approximately 40%.
- The overall economic burden of vision problems in the United States is estimated at $139 billion per year.
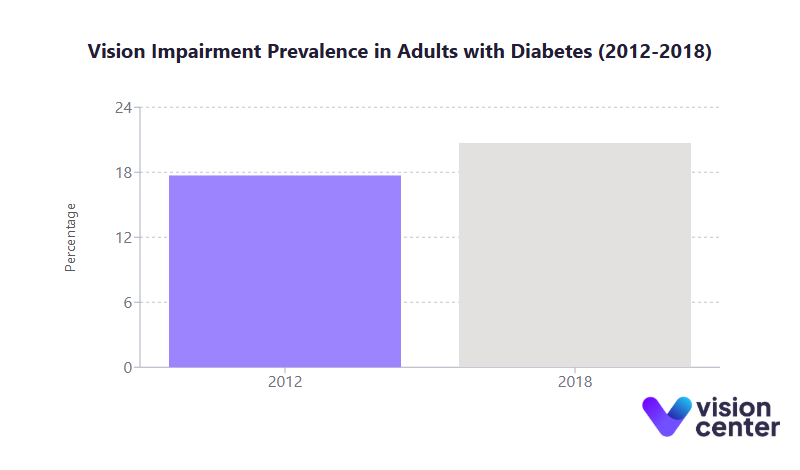
- Between 2012 and 2018, the prevalence of vision impairment in adults with diabetes increased from 17.7% to 20.7%.
Disease Correlation and Comorbidity Patterns
Understanding the correlation between chronic conditions and eye health is essential for identifying high-risk groups and tailoring preventative care.
- Diabetes:
- Approximately 29% of U.S. adults over 40 with diabetes suffer from diabetic retinopathy.
- Diabetic individuals experience nearly 1.6 times higher odds of vision impairment.
- Diabetes increases the risk of open-angle glaucoma and cataracts by making these conditions 2 to 5 times more likely.
- Hypertension:
- Chronic high blood pressure damages retinal blood vessels, contributing to hypertensive retinopathy.
- Older adults with hypertension have about 1.4 times higher odds of vision impairment.
- Uncontrolled hypertension not only threatens eye health but also signals potential damage to other vital organs.
- Cardiovascular Disease and Stroke:
- A history of stroke is associated with roughly 2 times higher odds of vision impairment in seniors.
- There is a marked prevalence of cardiovascular issues among adults with vision loss compared to those with normal vision.
- Chronic Kidney Disease and Other Conditions:
- Older adults with chronic kidney disease show a 2.3 times higher association with vision impairment.
- Conditions like arthritis and chronic lung disease often co-occur with eye health issues, further increasing the risk of vision loss.
Table 1. Eye Conditions Among U.S. Adults (45+) with Diabetes (2016–2017)
| Eye Condition | Prevalence in Adults 45+ with Diabetes | Vision Loss Due to Condition (in same group) |
| Cataracts | 32.2% | 9.2% |
| Diabetic Retinopathy | 8.6% | 4.1% |
| Glaucoma | 7.1% | 2.1% |
| Macular Degeneration | 4.3% | 2.2% |
This table underscores the significant burden of eye conditions among middle-aged and older adults with diabetes. It also illustrates how prolonged exposure to chronic disease factors can increase the likelihood of developing multiple ocular disorders.
Intervention Effectiveness and Prevention Programs
Assessing treatment effectiveness and preventive strategies is crucial for mitigating the impact of chronic conditions on eye health.
- Treatment Advances:
- Laser photocoagulation therapy can reduce the risk of severe vision loss in diabetic retinopathy by at least 60%.
- Anti-VEGF injections have significantly improved outcomes for diabetic macular edema and proliferative retinopathy.
- Timely cataract surgery effectively restores vision for patients whose condition was accelerated by chronic disease factors.
- Preventive Care and Screening:
- An estimated 90% of blindness in U.S. adults with diabetes is preventable through regular eye exams and proper care.
- Only about 54.1% of Medicare Part B beneficiaries with diabetes received an annual eye exam in 2017, revealing gaps in preventive screening.
- Telemedicine, such as teleretinal screening programs, has proven effective in increasing screening rates in underserved areas.
- Prevention Programs:
- The National Diabetes Prevention Program (NDPP) has helped over 750,000 high-risk adults achieve a 50 to 60% reduction in progression to type 2 diabetes.
- Diabetes Self-Management Education and Support (DSMES) services reach nearly 1 million people annually, lowering the risk of multiple complications, including vision loss, by about 40%.
These interventions demonstrate that the proactive management of chronic conditions and regular eye examinations can significantly improve vision outcomes and reduce the incidence of severe ocular complications.
Healthcare Utilization and Cost Burden
The intersection of chronic diseases and eye health creates substantial challenges for healthcare systems, both in service delivery and economic terms.
- Economic Impact:
- Diabetes-related complications, including eye disorders, account for nearly 48% to 64% of a diabetic person’s lifetime medical costs.
- The overall economic burden of vision problems, including treatment and productivity losses, is estimated at $139 billion per year.
- Annual costs related to blindness, including disability payments and lost taxable income, can reach approximately $11,900 per affected individual.
- Service Utilization:
- Patients with diabetes and advanced retinopathy require frequent specialist visits, ranging from quarterly endocrinology check-ups to regular dilated eye exams.
- Lifelong management of conditions like glaucoma often necessitates ongoing medication, laser therapy, or surgical interventions.
- More than 60% of diabetes-related healthcare costs are incurred by adults aged 65 and older, highlighting the heavy burden on Medicare and Medicaid systems.
- Access to Care:
- Over half of American adults delay or skip routine eye care due to cost barriers or a lack of awareness about the need for regular check-ups.
- Racial, ethnic, and geographic disparities exist in eye exam uptake, with white Medicare beneficiaries more likely to receive annual eye exams compared to Black and Hispanic beneficiaries.
- Rural regions, particularly in the Southeast and Appalachian areas, face higher rates of chronic disease and fewer eye care providers, further exacerbating vision health disparities.
These statistics reveal the dual challenge of high utilization and significant cost burdens that strain both patients and healthcare systems, underlining the importance of efficient resource allocation and improved access to preventive services.
Patient Outcomes and Long-Term Trends
Evaluating patient outcomes and long-term trends offers critical insights into the broader implications of chronic conditions on quality of life and future healthcare challenges.
- Quality of Life:
- Vision loss often leads to reduced independence and daily functioning, affecting activities such as reading, driving, and self-care.
- Nearly 25% of adults with vision loss report experiencing symptoms of anxiety or depression.
- Younger adults with vision impairment face nearly 5 times the risk of serious psychological distress compared to their older counterparts, emphasizing the social and economic costs of early vision loss.
- Age Group Distribution:
- Approximately 12 million people aged 40 and older in the U.S. have some form of vision impairment.
- This number is projected to more than double by 2050 due to an aging population and increased chronic disease prevalence.
- While children and young adults are less affected, rising rates of childhood obesity and type 2 diabetes signal emerging concerns for early-onset diabetic retinopathy.
- Geographic Variation and Trends:
- Diabetic retinopathy prevalence varies by state, ranging from about 20.8% in Nevada to 31.3% in Massachusetts.
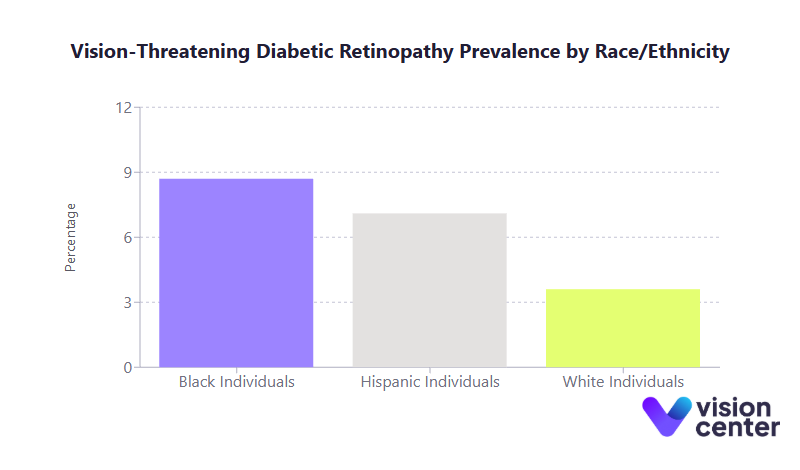
- Racial and ethnic disparities are pronounced; for example, vision-threatening diabetic retinopathy affects approximately 8.7% of Black individuals and 7.1% of Hispanics, compared to 3.6% in white individuals.
- Long-term trends show a plateau, and in some cases a slight uptick, in vision impairment among diabetic adults after years of decline, indicating that further reductions in vision loss may require new strategies and innovations.
These findings highlight the profound impact of chronic conditions on patient quality of life and the need for sustained public health efforts. They also underscore the importance of targeted interventions that address not only medical treatment but also broader social and economic determinants of health.
As we reflect on the data presented, it is clear that chronic conditions exert a considerable toll on eye health, affecting millions of Americans. The interplay between systemic diseases and ocular complications requires an integrated approach that combines effective medical treatment, regular screening, and robust preventive programs. Addressing disparities in healthcare access and ensuring that high-risk populations receive timely interventions remain critical priorities.
The long-term implications of these trends are far-reaching. As the U.S. population continues to age and chronic disease prevalence increases, healthcare systems must adapt to meet growing demands. Ultimately, improving eye health outcomes will not only enhance the quality of life for affected individuals but also alleviate the economic strain on public health resources by reducing the burden of advanced disease and its associated costs.
In this article
5 sources cited
Updated on March 25, 2025
Updated on March 25, 2025
About Our Contributors
Mara Sugue, with a B.A. in Social Sciences, is a dedicated web content writer for Vision Center. She is committed to making eye health research accessible and understandable to people from diverse backgrounds and educational levels. Her writing aims to bridge the gap between complex vision health topics and readers' needs for clear, factual information.
Dr. Melody Huang is an optometrist and freelance health writer with a passion for educating people about eye health. With her unique blend of clinical expertise and writing skills, Dr. Huang seeks to guide individuals towards healthier and happier lives. Her interests extend to Eastern medicine and integrative healthcare approaches. Outside of work, she enjoys exploring new skincare products, experimenting with food recipes, and spending time with her adopted cats.

